Nephrology: Clinical
Nephrology 1: AKI
248 - Outcomes of Acute Kidney Injury Recovery Phenotypes in Non-ICU Pediatric Hospital Admissions
Publication Number: 248.25
- AB
Abby M. Basalely, MD, MS (she/her/hers)
Assistant Professor
Cohen Children's Medical Center
West Hempstead, New York, United States
Presenting Author(s)
Background:
Longer AKI recovery in adults and critically ill children is associated with poor short and long-term outcomes. Majority (65%) of pediatric AKI occurs outside the ICU; however, associations of AKI recovery patterns in noncritically ill pediatric patients with outcomes are unknown.
Objective:
Determine the association of AKI development and recovery phenotypes with admission diagnoses, average gross hospital cost, and LOS in noncritically ill children
Design/Methods: A retrospective analysis of children 1mo-21 years with >2 serum creatinine values, admitted to 3 pediatric hospitals January 2012-December 2020 was performed. AKI was defined using KDIGO serum creatinine criteria. The first AKI episode of an admission was evaluated. Patients with LOS < 48 hours(h), chronic kidney disease, dialysis dependence, kidney transplant, pregnancy, or admission to the ICU were excluded. Exposures were AKI development and recovery phenotypes, classified as (1) Transient AKI (tAKI), resolved within 48h, (2) Persistent AKI (pAKI), AKI >48h & < 7 days(d), or (3) Acute Kidney Disease (AKD), AKI >7d. Outcomes included LOS(d) & gross hospital costs($).
Results:
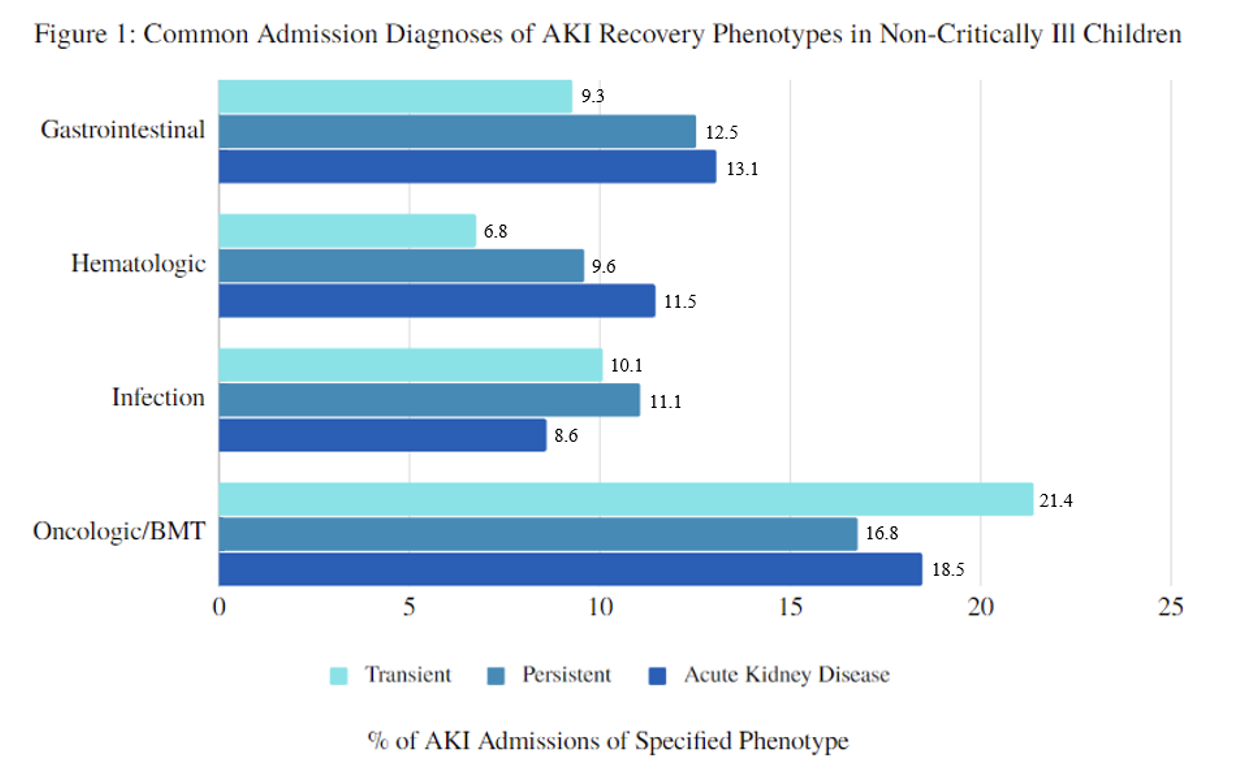
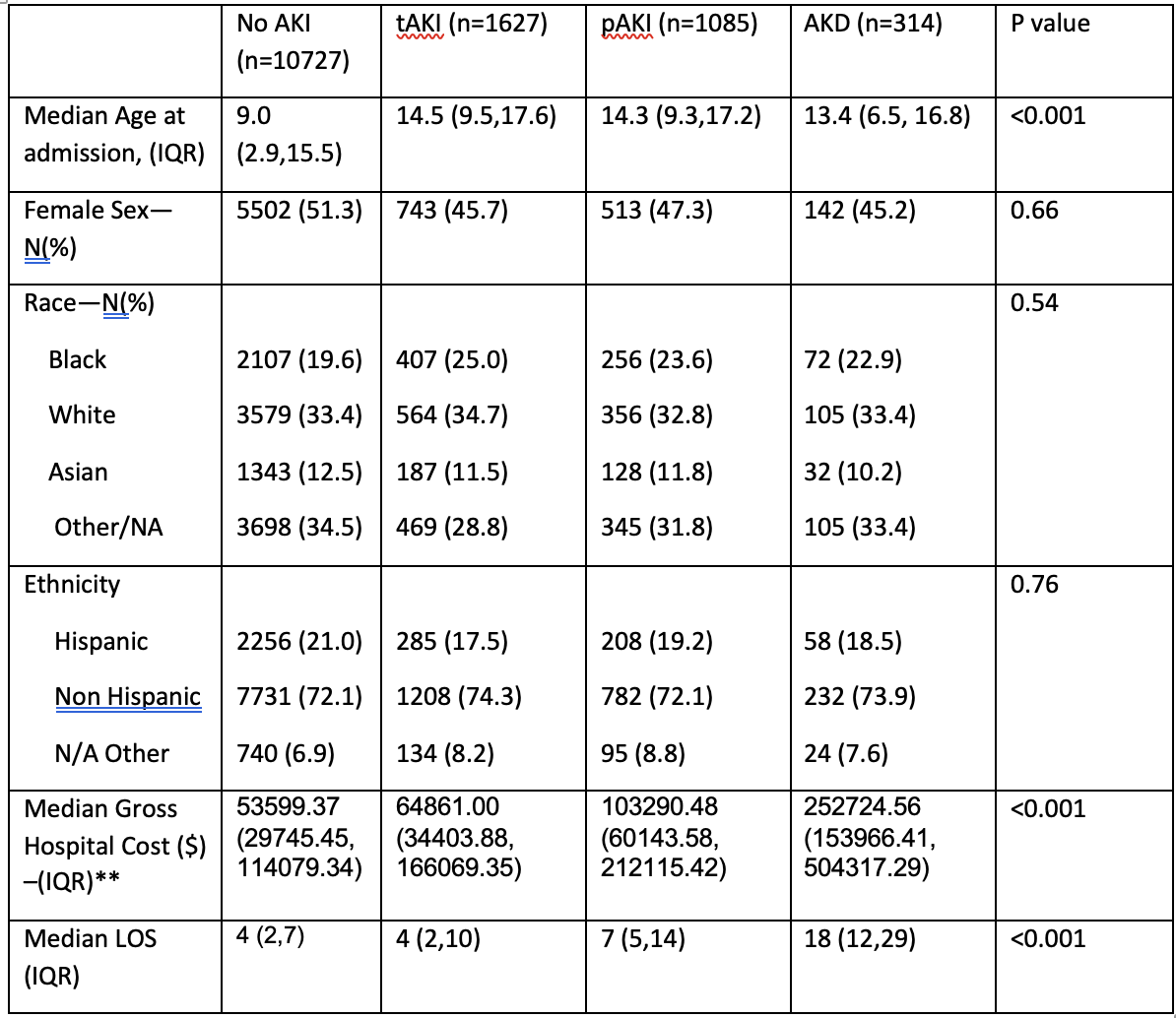
AKI developed in 24.3% (N=3026) of all admissions (N=12,445). Median LOS was 3d greater in children with AKI vs no AKI [median (IQR) 7(4,15) vs 4(2,7), p< 0.001]. Financial data was available for 12,089 admissions, and 2,670 had AKI. Median gross costs were $42,000 greater for children with vs without AKI ($95,876 vs $53,599, p< 0.001). There were no significant differences among AKI recovery phenotypes in sex, race, and ethnicity (Table 1). AKD occurred in children who were younger [13.4(6.5,16.8)] vs tAKI [14.5(9.5, 17.6)] or pAKI [14.3(9.3, 17.2)], p< 0.001. The most common phenotype was tAKI (N=1,627, 53.7%) which was most common in oncologic/bone marrow transplants (BMT) and infectious disease admissions. AKD occurred in 10.4% (N=314) of phenotypes and was most common in gastrointestinal and oncologic/BMT diagnoses. Median gross hospital cost was significantly greatest in AKD ($252,724) vs pAKI ($103,290) vs tAKI ($64,861) p< 0.001. Similarly, median LOS was longest in AKD [18d (12,29)] vs pAKI [7d, (5,14)] vs tAKI [4d (2,10)].
Conclusion(s):
This is the first study to characterize associations of pediatric AKI recovery phenotypes in non-ICU hospitalizations. These data suggest that hospital resources are taxed significantly by AKI in noncritically ill patients and more pronounced in those with prolonged AKI recovery. Further adjusted analyses are necessary to better characterize these patients and identify patients who would benefit from close follow-up care.