Neonatal General
Neonatal General 6: Neurology
708 - Comparison of cerebral blood flow and cerebral oxygenation measured non-invasively in extremely premature infants
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 708
Publication Number: 708.234
Publication Number: 708.234
John Sunwoo, Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Boston, MA, United States; Alyssa Martin, Massachusetts General Brigham, Charlestown, MA, United States; Sarah Lee, Harvard Medical School, Boston, MA, United States; Katie Hannon, Brigham and Women's Hospital, Boston, MA, United States; Tina Steele, Brigham and Women's Hospital, North Billerica, MA, United States; Deborah Cuddyer, Brigham and Women's Hospital, Braintree, MA, United States; Emily M. Herzberg, Mass General For Children, Lynnfield, MA, United States; Terrie Inder, Childrens Hospital of orange county, Irvine, CA, United States; Maria Angela Franceschini, Massachusetts General Hospital, Charlestown, MA, United States; Mohamed El-Dib, Harvard Medical School, Boston, MA, United States

John Sunwoo, PhD (he/him/his)
Research Fellow
Martinos Center for Biomedical Imaging, Massachusetts General Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Fluctuation in cerebral blood flow (CBF) in extremely preterm infants is a major risk for brain injury such as germinal matrix and intraventricular hemorrhage (GM/IVH). With the increasing availability of commercial near-infrared spectroscopy (NIRS) devices, many investigators have used cerebral tissue saturation (rSO2) as a surrogate for CBF. While the relationship between CBF and rSO2 has been studied and modeled in adults and animals, information is lacking in the extremely preterm infant population.
Objective: The aim of this study was to evaluate the relationship (i.e. the signal similarity quantified by cross-correlation) between CBF and rSO2, measured using diffuse correlation spectroscopy (DCS) and clinical NIRS, respectively, in extremely low gestational age newborns (ELGA, < 29 weeks gestation). In addition, we investigated the possible association with different GM/IVH outcomes.
Design/Methods: We recruited ELGA newborns in the Brigham and Women’s Hospital NICU and monitored the infants for 3-6 hours a day for 3 consecutive days starting within 48 hours after birth. We continuously monitored cerebral and scalp blood flow (SBF) via a custom DCS system and cerebral oxygenation via clinical NIRS (INVOS). Additional vital parameters, including heart rate, arterial oxygen saturation (SpO2), and if available, mean arterial pressure (MAP) and transcutaneous pCO2 were co-recorded. All signals were resampled to 0.03 Hz to match the native sampling rate of our NIRS device. We obtained sets of Spearman’s correlation (R) at their best time lag (Tr, within ±3 minutes) using a 30-minute sliding window on all signal pairs.
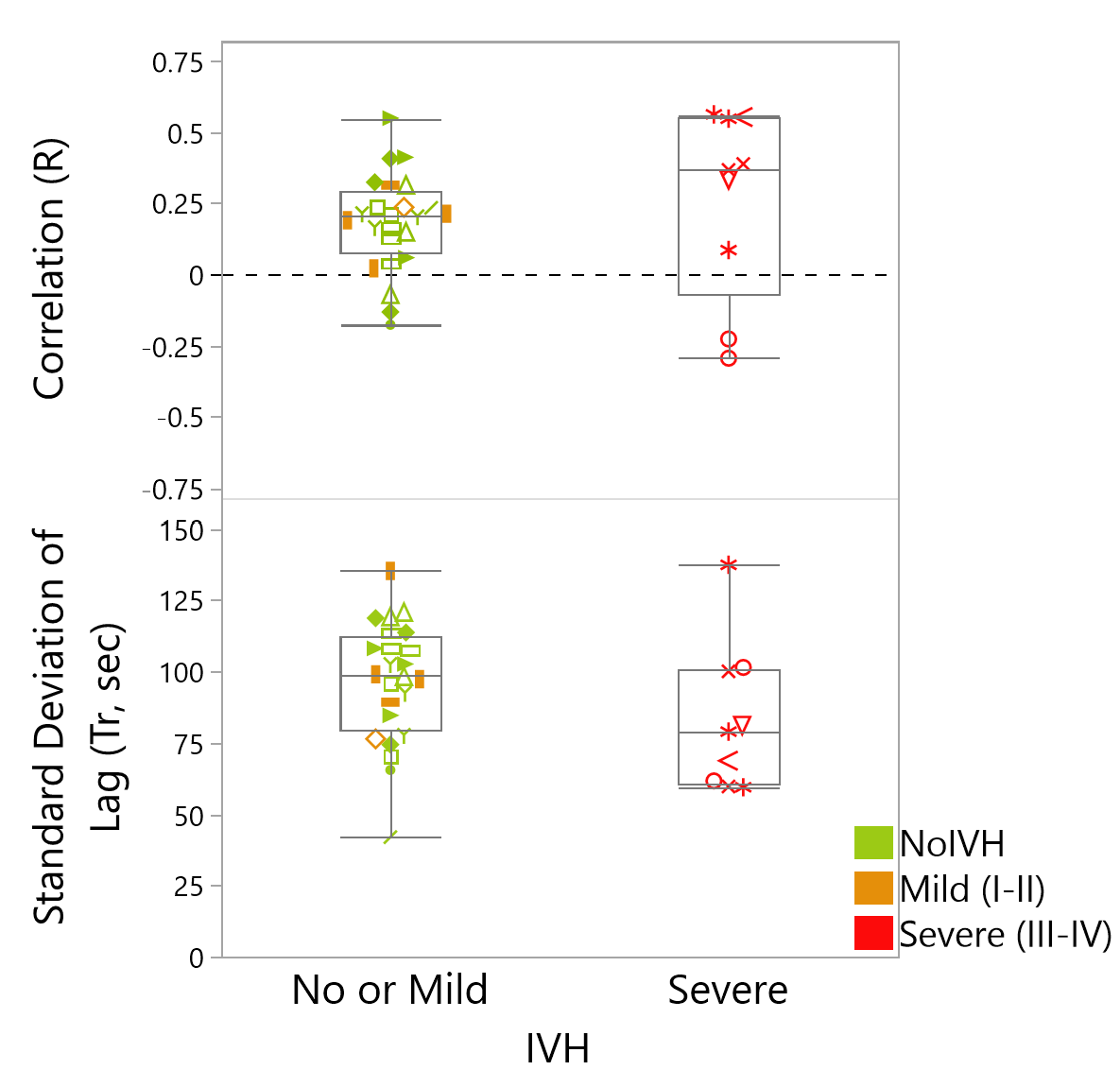
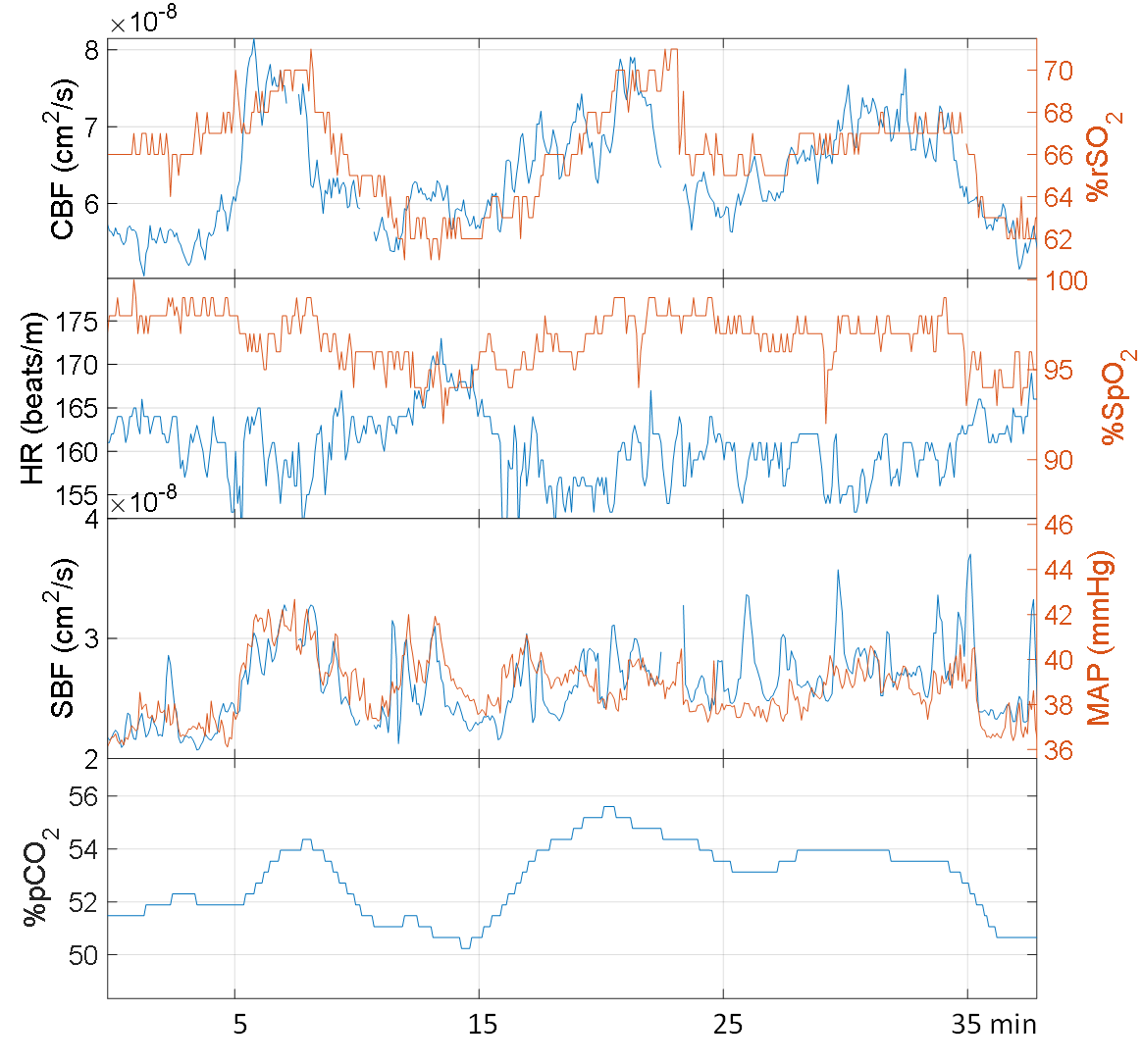
Results: Sixteen ELGA infants were included in the analysis, resulting in 33 daily monitoring sessions (Table 1). In all subjects, the mean ± standard deviation of correlation coefficients was 0.20±0.42, with Tr of 30±93 seconds, suggesting a positive but weak correlation between CBF and rSO2. These metrics did not seem significantly different in the severe IVH group (defined as IVH grade >II), although, a slightly tighter variation in Tr was trended with severe IVH (P=.13, Fig.1). Fig. 2 illustrates a 30-minute window of a strong correlation between CBF and rSO2 (R=0.72), along with the rest of the co-recorded measurements in a 24-week GA infant who was diagnosed with a grade-IV IVH.
Conclusion(s): While there is a relation between CBF and rSO2, investigators should be cautious about using them interchangeably. We are currently finalizing data analysis using the co-registered vital measurements to get a comprehensive summary of this population in the context of their clinical outcomes.
.png)