Neonatal-Perinatal Health Care Delivery: Practices and Procedures
Neonatal-Perinatal Health Care Delivery 3: Practices: Growth & Nutrition, Potpourri
762 - Effect of visual inspection based abdominal monitoring versus routine pre-feed abdominal girth monitoring on time to reach full enteral feeds in preterm neonates: A randomized controlled trial
Publication Number: 762.247

Vivek Kumar, MD. DM (he/him/his)
Research Consultant
AIIMS New Delhi
New Delhi, Delhi, India
Presenting Author(s)
Background: Routine pre-feed abdominal girth monitoring or gastric residual volume measurement is used to define feed intolerance in neonates, the evidence for which is sparse.
Objective:
To compare the effect of visual inspection-based abdominal monitoring (VI) with routine pre-feed abdominal girth monitoring (AG) to detect feed intolerance on time to reach full enteral feeding in preterm neonates.
Design/Methods:
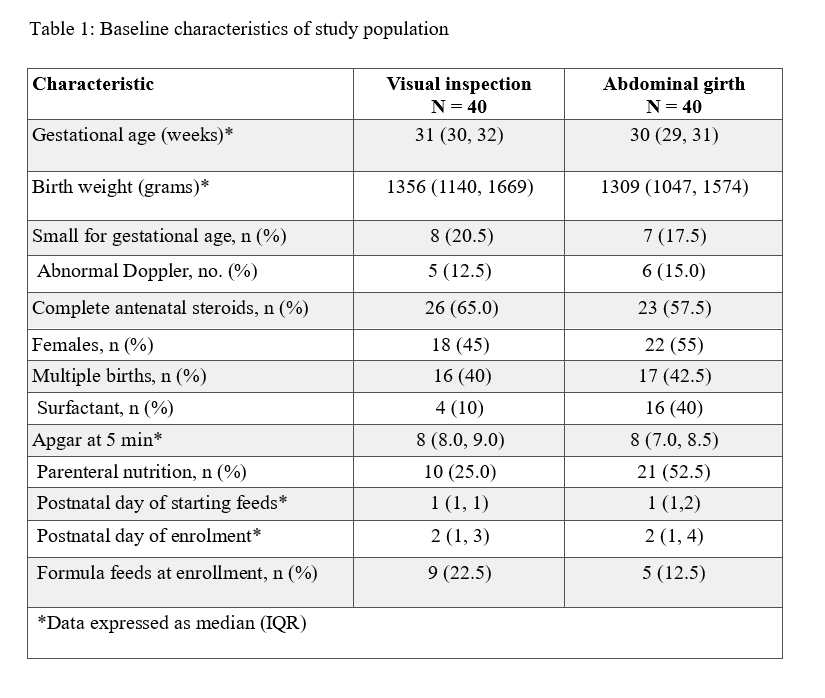
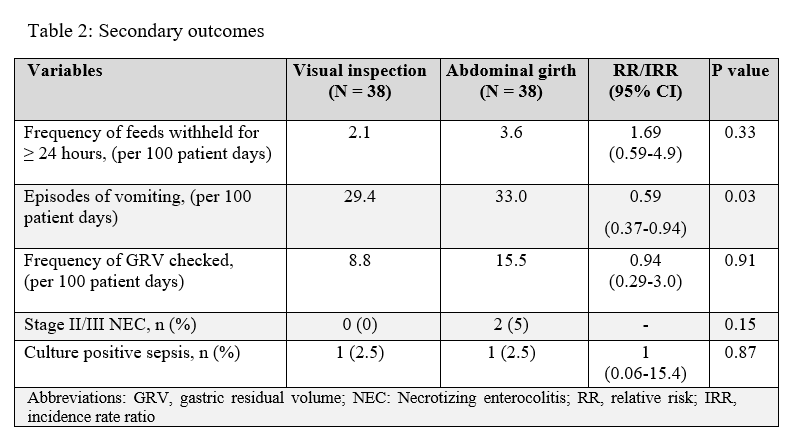
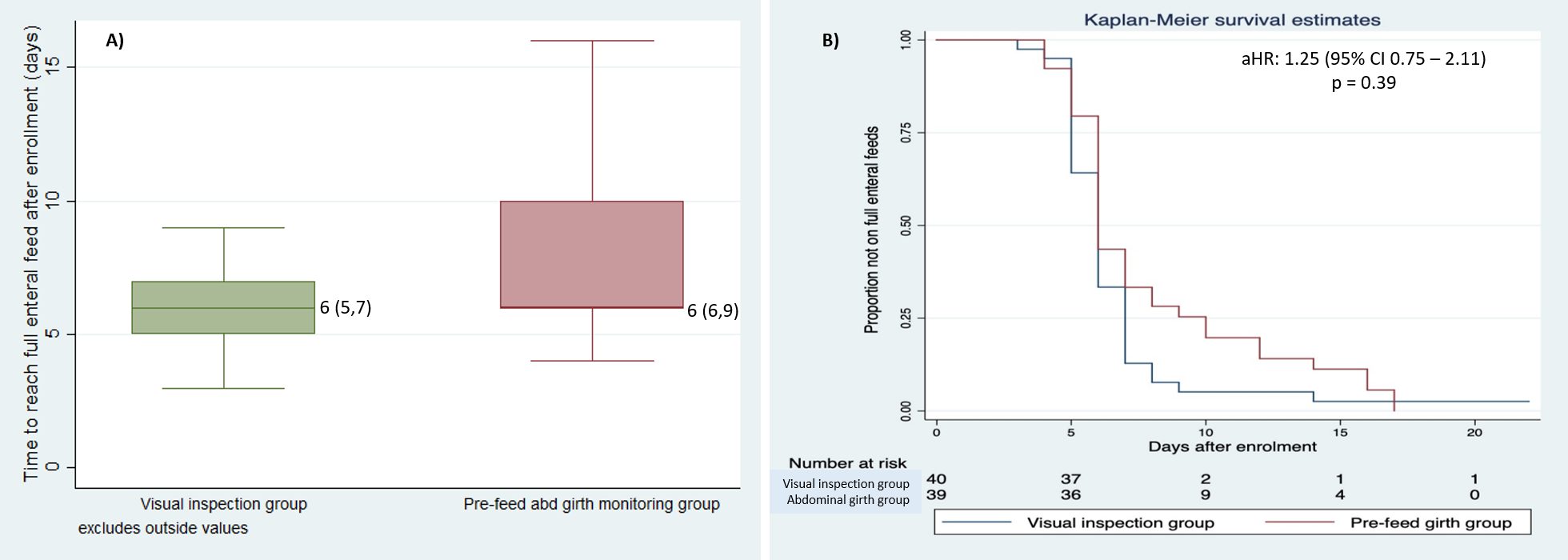
This randomized trial was conducted in inborn neonates born at or before 32 weeks’ gestation at a level-3 NICU in India. Eligible neonates receiving at least 30 mL/kg/day enteral feeds were randomized to the VI or AG groups. Neonates in the former group were assessed for the presence of obvious abdominal distension, >2 visible intestinal loops, or shiny/tense/erythematous abdominal wall by visual inspection. Pre-feed abdominal girth was measured routinely in the neonates in the AG group. The primary outcome was time to reach enteral feeds of at least 150 mL/kg/day. Secondary outcomes were the frequency of withholding feeds for at least 24 hours and vomiting, the incidence of stage II/III NEC and culture-positive sepsis, and weekly weight gain till hospital discharge.
Results:
A total of 80 neonates were randomized to the VI (n= 40) or AG (n= 40) groups. A higher proportion of neonates received surfactant (40% vs 10%) and parenteral nutrition (52.5% vs 25%) in the AG group (table 1). There was no difference in the time to reach full feeds after adjusting for baseline imbalances (median [IQR] 6 [5-7] vs. 6 [6-9] days, respectively; adjusted hazard ratio: 1.25; 95%CI 0.75 to 2.1) (figure 1). The frequency of withholding feeds for 24 hours was comparable (2.1 vs. 3.6 per 100 patient-days; incidence rate ratio [IRR] 1.69; 95% CI 0.59 to 4.9). However, the incidence rate of vomiting was significantly lower in the VI group (29.4 vs. 33.0 per 100 patient days; IRR 0.59; 95% CI 0.37 to 0.94). There were no differences in other secondary outcomes (table 2).
Conclusion(s): Visual inspection-based selective abdominal monitoring for feed intolerance did not affect the time to reach full enteral feeds but reduced the incidence rate of vomiting. If confirmed in large trials, the results might help change the practice of routine pre-feed abdominal girth monitoring for feed intolerance, thus preventing unnecessary handling of preterm neonates.