Neonatal General
Neonatal General 5: COVID, Infections Diseases
693 - Incidence of prematurity before and during COVID-19 lockdown in a tertiary hospital.
Publication Number: 693.233

Roberta Bravo Quintans, MD (she/her/hers)
neonatology fellow
Hospital Italiano de Buenos Aires
CABA, Ciudad Autonoma de Buenos Aires, Argentina
Presenting Author(s)
Background:
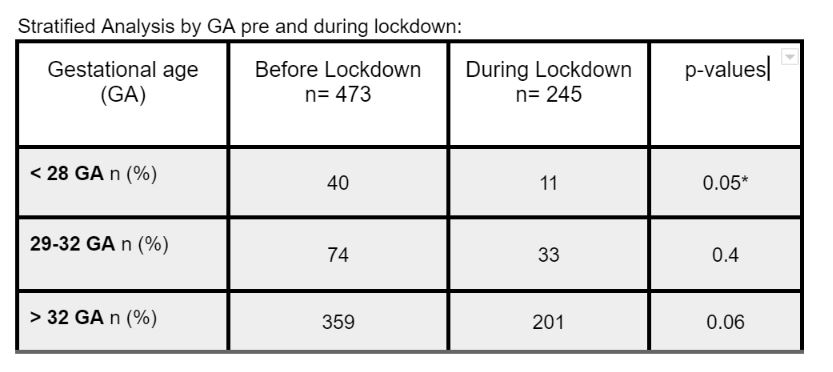
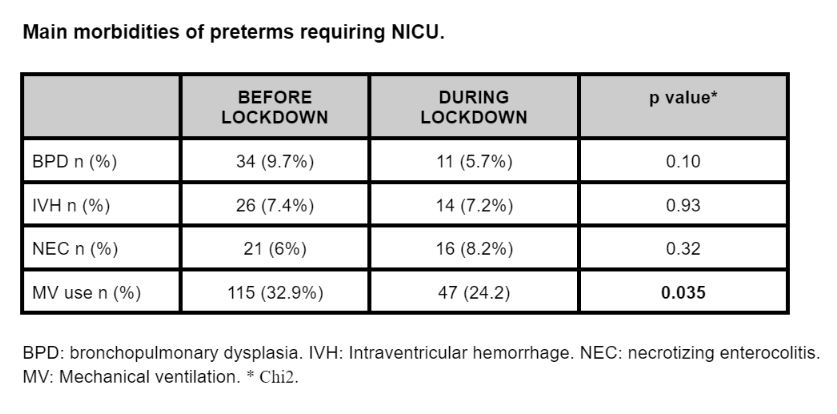
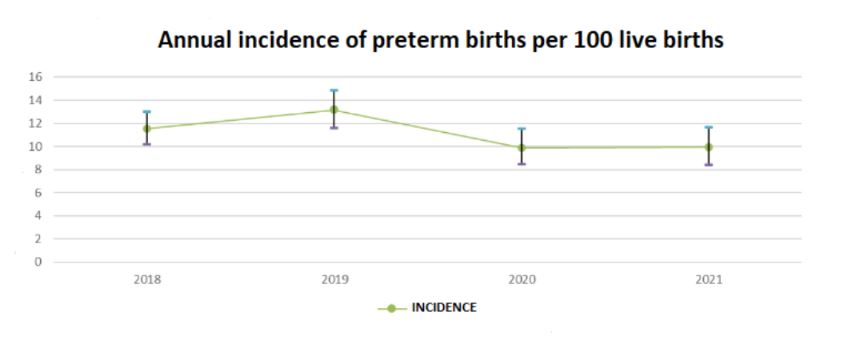
COVID-19 infection could be a risk factor for preterm births. Widespread lockdown during COVID-19 pandemic could have affected birth outcomes worldwide. On March 20th the Argentine government declared a COVID-19 lockdown. Since then, its association with the incidence of preterm births has been controversial. The estimated worldwide rate of prematurity is 10.4% and its etiology is multifactorial (social, obstetric, fetal, environmental, etc.) so relatively few cases of preterm birth can be prevented using current strategies. 6364 inborn children were included in the study period, of those 718 were preterm babies (11.2%). The total number of newborns in the pre-lockdown epoch was 3599, out of which, 473 (13%) were preterms. During the lockdown, there were 2765, out of which 245 (9.98%) were preterms. Baseline characteristics were similar between epochs (birth weight, sex, IUGR, gestational diabetes) except maternal hypertension: 13.3% pre lockdown vs 20.8% during lockdown (p=0,009). The annual incidences of prematurity were similar: 11% (95% CI 10.17-13.02) in 2018, 13% (95% CI 11.63-14.87) in 2019, 9% (95% CI 8.48-11.54) in 2020, and 9% (95% CI 8.41-11.66) in 2021. Comparing epochs, the incidence of prematurity was significantly higher pre-lockdown, 12.28% (95% CI 11.25-13.39), than during lockdown, 9.90% (95% CI 8.82-11.08) (p=0.003). In the stratified analysis by GA, the frequency of prematurity cases under 28 wk decreased by 56% during COVID-19 lockdown compared to the previous epoch (p=0.05). Admission to the NICU was significantly lower in the pre-lockdown epoch, 74%, than during COVID-19 lockdown, 79.8% (p=< 0.001). In regards to morbidities, the use of mechanical ventilation decreased during lockdown by 24.2% compared to the previous epoch of 32.9% (p=0.035)
Objective: 1) To estimate and compare the incidence of prematurity between two epochs: 2018 to 2019 (pre-lockdown), and 2020 to 2021 (during lockdown) 2) To compare NICU admissions and describe the most important morbidities pre and during COVID-19 lockdown
Design/Methods: Retrospective study, before and during COVID-19 lockdown in a cohort of inborn under 36 wk gestational age (GA). Baseline characteristics of each group, annual incidence of prematurity, admission to the NICU and morbidities associated with the corresponding epoch were analyzed with univariate analysis. Then, the frequencies of prematurity cases were compared between epochs, stratified by GA
Results:
Conclusion(s): According to our study, there was a decrease in the incidence of prematurity during COVID-19 lockdown, particularly significant under 28 wk GA