Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 2
530 - Evidence for Stigmatizing Language in the Medical Record Perpetuating Race-Based Biases
Publication Number: 530.117

Brittany C. Kimball, MD (she/her/hers)
Chief Resident
University of Minnesota Medical School
Minneapolis, Minnesota, United States
Presenting Author(s)
Background:
Electronic medical records (EMR) convey robust medical data but can also be burdened by note writers’ biases. Stigmatizing language pervades the EMR with varying degrees of medical relevance. Excess workload can also lead to documentation shortcuts, including copy-forwarding, which can perpetuate stigma.
Objective:
We investigated whether certain stigmatizing terms in the EMR are used equitably across demographics with three hypotheses in mind: 1) Negative terminology is used more frequently in underrepresented minority groups, 2) Words with shock value (such as specific curse words) are used more frequently than more general descriptors of these terms (e.g. “cursing”), and 3) “compliant” or “noncompliant” descriptors rarely change for an individual.
Design/Methods:
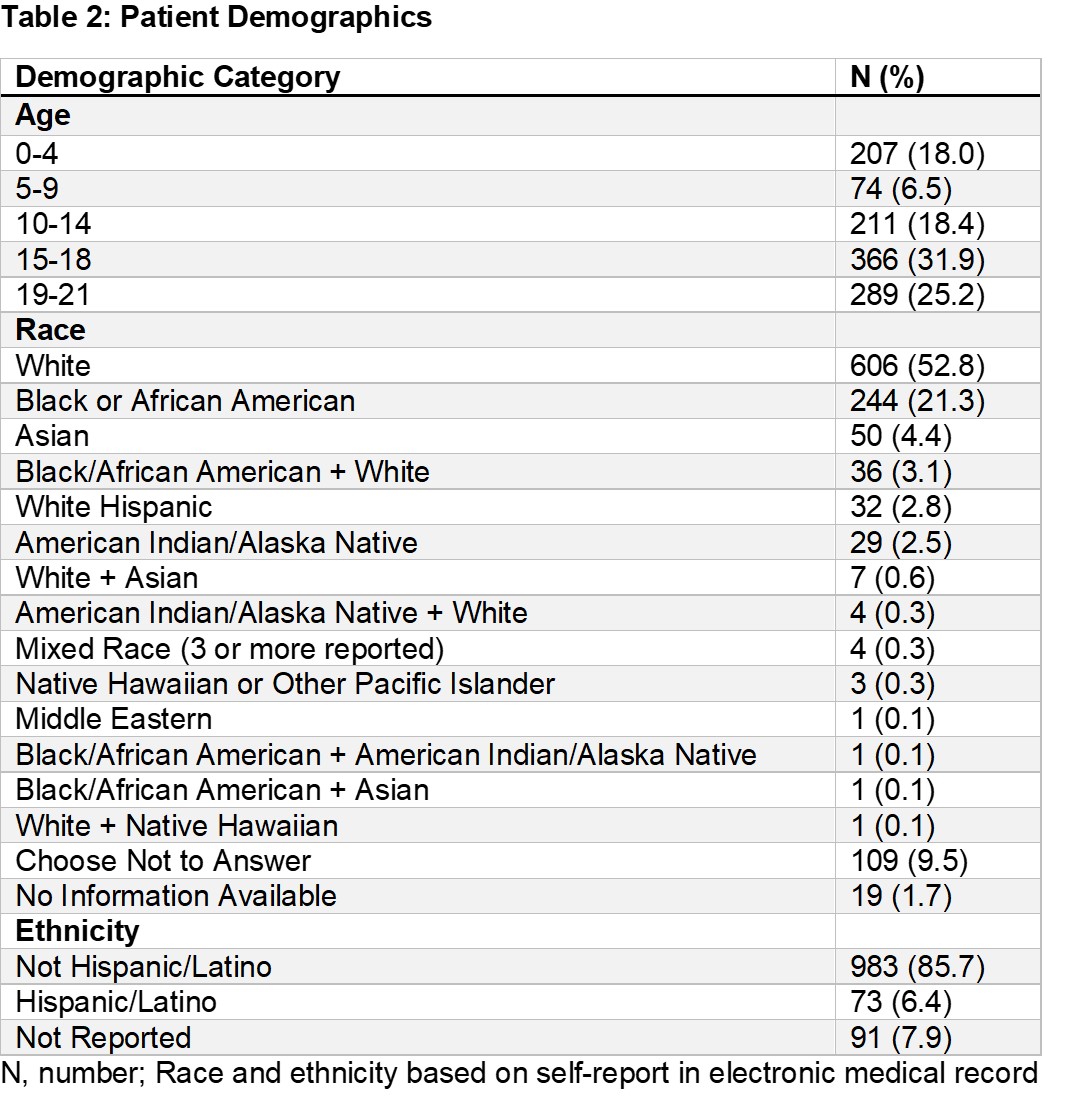
Using natural language processing software, inpatient and emergency department notes from a large health system from 1/1/2019 – 6/30/21 were analyzed. Encounters were for patients aged 0-21 years (caregivers may be described) with one encounter/patient if they contained ≥1 of a set of positive and/or negative terms (Table 1). Authors’ manual data review confirmed appropriate use of terms. Odds ratios (OR) and 95% confidence intervals (CI) were calculated for race comparisons. P</span>≤0.05 was considered significant. Table 2 shows demographics. Race comparisons were limited to White Non-Hispanic vs Black/African-American due to cohort’s racial makeup. A total of 1315 encounters (1147 individuals) were reviewed. Median age was 15 years (interquartile range 10 – 19 years). Negative terms were more prevalent than positive ones (n=840 vs 589) though no strong race trends were seen; multiple positive search terms had too few events to analyze. “Compliant” was seen more than twice as often as “noncompliant” (n=287 vs 128), yet “noncompliant” was used more for Black patients than White ones (OR 1.45; 0.92, 2.26; p=0.09), a trend not seen with “compliant”. “Noncompliant” or “compliant” were seen on an encounter’s initial date in 84% and 80% of occurrences, respectively. Switches from “noncompliant” to “compliant” and vice versa were rare but occurred equally in both directions. Specific curse words were noted twice as often as “cursing” or profanity”. “Cursing"/"profanity” and “disrespectful” showed modest non-statistically significant race-based trends (Table 3). Negative descriptors abound in the EMR even if medical relevance is limited or absent. This type of stigmatizing language risks further enhancing health inequities by ossifying patient characterizations that may be colored by healthcare provider biases.
Results:
Conclusion(s): .jpg)
.jpg)
