Critical Care
Critical Care 1
4 - Changes in Bronchiolitis Incidence and Ventilation Practices in 2020-22 Compared with 2010-2019
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 4
Publication Number: 4.107
Publication Number: 4.107
Jonathan H. Pelletier, Akron Children's Hospital, Akron, OH, United States; Ryan Nofziger, Akron Children's Hospital, Akron, OH, United States; Christopher Page-Goertz, Akron Children's Hospital, Hudson, OH, United States; Bryan P. McKee, Akron Children's Hospital, Akron, OH, United States; James Besunder, Akron Children's Hospital, Akron, OH, United States; Brittany Potts, Akron Children's Hospital, Akron, OH, United States; Christopher Horvat, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Michael L. Forbes, Akron Children's Hospital, Akron, OH, United States

Jonathan H. Pelletier, MD (he/him/his)
Pediatric Intensivist
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background: The COVID-19 pandemic resulted in social distancing measures, mask mandates, and school closures, with an accompanying decrease in pediatric respiratory admissions. The lasting effects on respiratory virus seasonality remain unexplored.
Objective: To compare changes in bronchiolitis seasonality as well as ventilation practices between the beginning of the COVID-19 pandemic and the decade prior.
Design/Methods: Retrospective, cross-sectional study of the Pediatric Health Information Systems database including children < 24 months old admitted with bronchiolitis between 06/01/2010 and 10/31/2022. Patients with complex chronic conditions were excluded. Admissions and ventilation practices were described with summary statistics. Non-invasive ventilation, including high flow cannula, (NIV) failure was defined as use of invasive mechanical ventilation (IMV) after use of NIV. Admissions were transformed into time series data and ensemble forecasting models were generated to analyze monthly admissions beginning 7/2020 compared to previous bronchiolitis seasons.
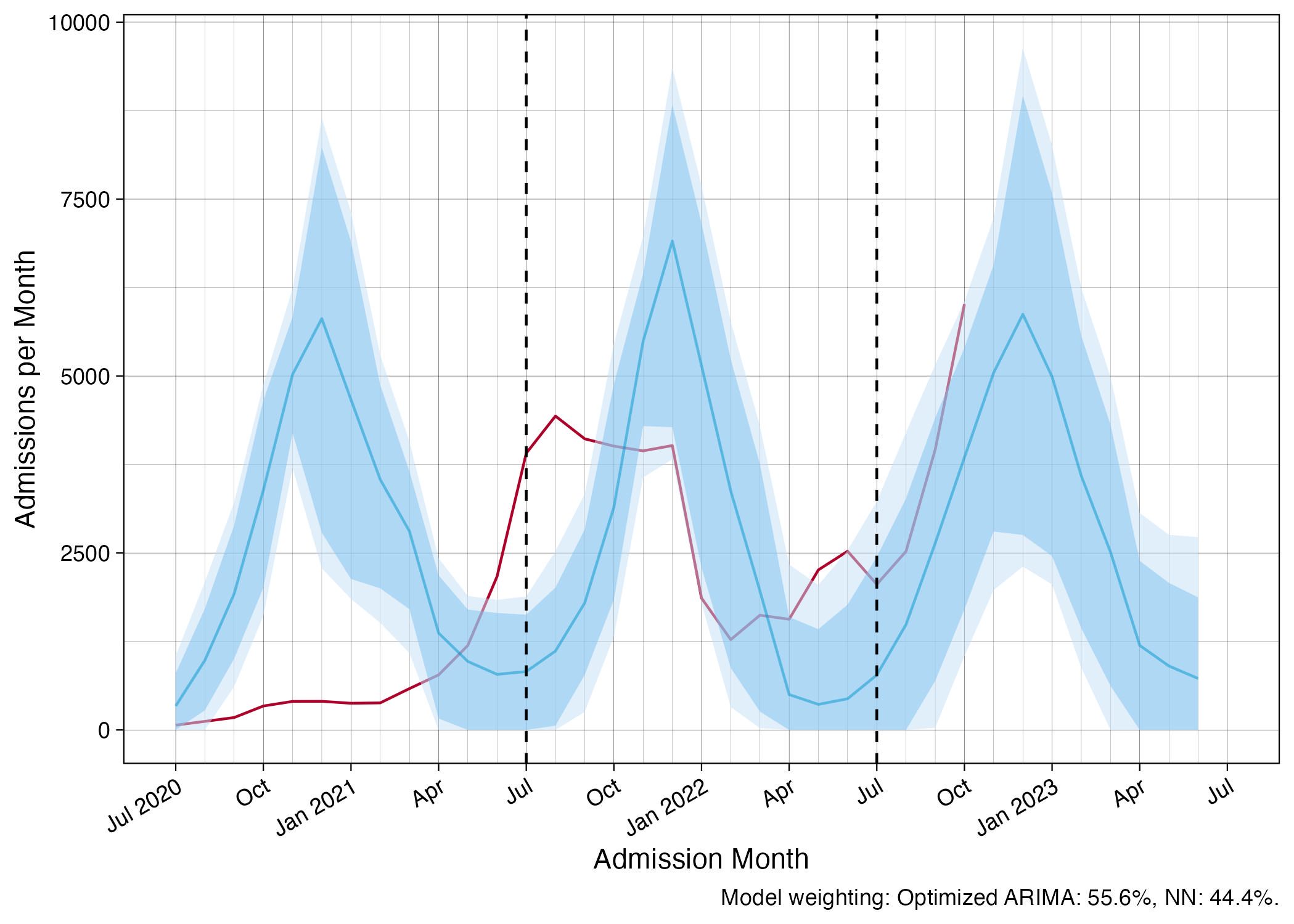
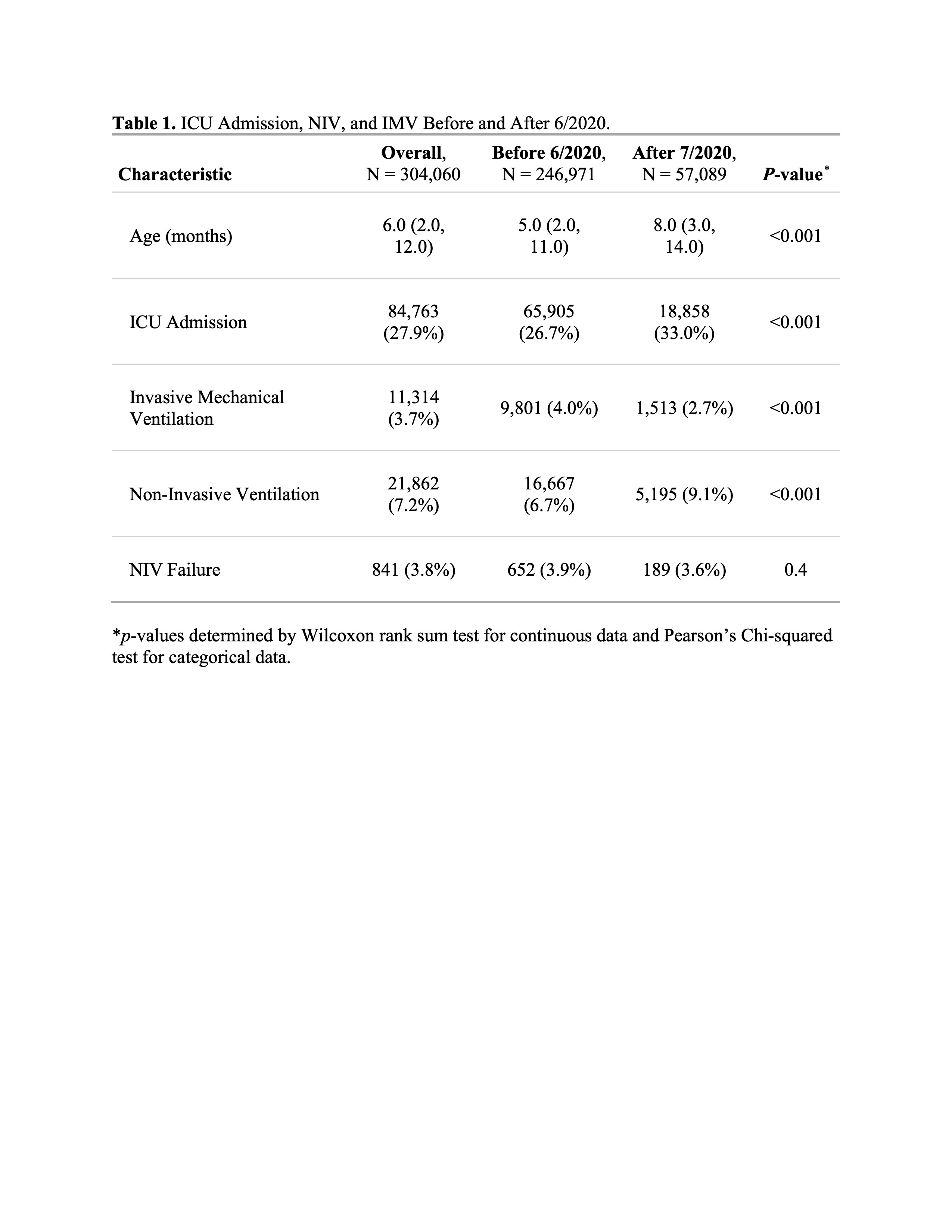
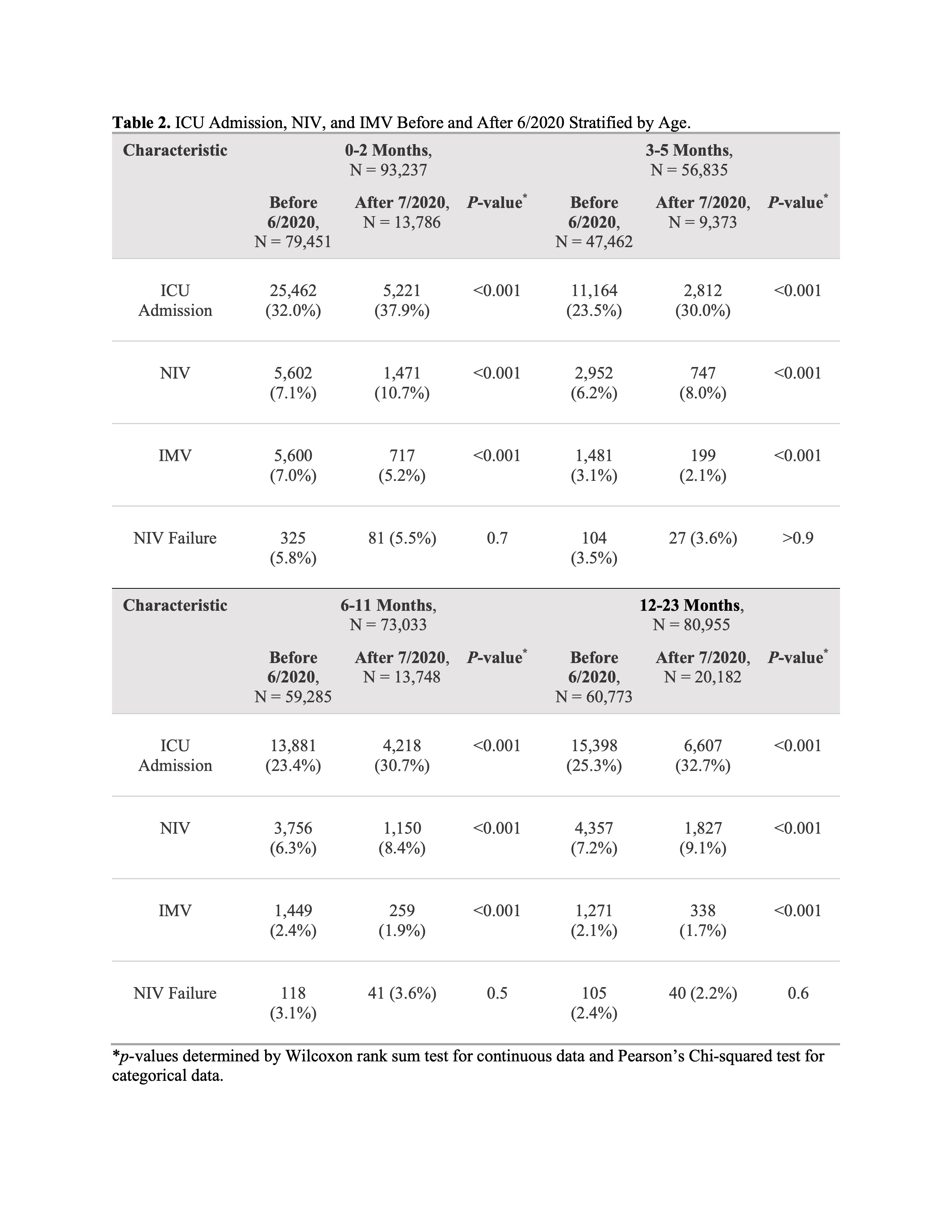
Results: There were 304,060 bronchiolitis admissions among 276,531 patients across 44 hospitals. There were 6,992 admissions between 7/2020-6/2021 compared to 32,960 [95% CI 14,529-51,397] predicted. There were 35,539 admissions between 7/2021-6/2022 compared with 32,537 [95% CI 11,478-58,733] predicted, but with an atypical seasonal distribution, peaking in 8/2021. There were 14,558 admissions between 7/2022-10/2022 compared to 8,189 [95% CI 1,074-19,698] predicted, with an earlier seasonal rise in admissions (Figure 1). Compared to before 6/2020, patients admitted after 7/2020 were older (median [IQR] age 8 [3-14] versus 5 [2-11] months, p < 0.001), more likely to be admitted to an intensive care unit (ICU; 33.0% [18,858/57,089] versus 26.7% [65,905/246,971], p < 0.001), more likely to receive NIV (9.1% [5,195/57,089] versus 6.7% [16,667/246,971], p < 0.001), and less likely to receive IMV (2.7% [1,513/57,089] versus 4.0% [9,801/246,971], p < 0.001) (Table 1). Rates of NIV failure were not significantly different before and after 6/2020 in any age strata (Table 2).
Conclusion(s): Bronchiolitis admissions occurred earlier in the calendar year since the COVID-19 pandemic. Children admitted since the pandemic are older, more likely to be admitted to the ICU and more likely to receive NIV. Unlike prior studies, they were also less likely to receive IMV across all age strata. Further study is needed to identify characteristics of patients for whom NIV obviates the need for IMV.