Medical Education: Fellow
Medical Education 3: Fellow 1
492 - Pediatric Emergency Medicine Fellows’ (PEM) Training to Become Bedside Teachers: A National Survey of PEM Program Directors and PEM Fellows
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 492
Publication Number: 492.124
Publication Number: 492.124
David Kling, Nationwide Children's Hospital, Columbus, OH, United States; Maya S. Iyer, Nationwide Children's Hospital, Columbus, OH, United States; Sara Helwig, Nationwide Children's Hospital, Columbus, OH, United States
David Kling, Jr., DO (he/him/his)
Fellow
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: The pediatric emergency department is a unique and challenging learning environment. Educators require specific bedside teaching skills to enhance learners’ experiences, however teaching how to become a bedside teacher is not standardized.
Objective: We sought to 1) assess if Pediatric Emergency Medicine (PEM) fellowship programs have a dedicated curriculum to train their fellows to become bedside teachers 2) and if so, how do these programs measure curricular effectiveness?
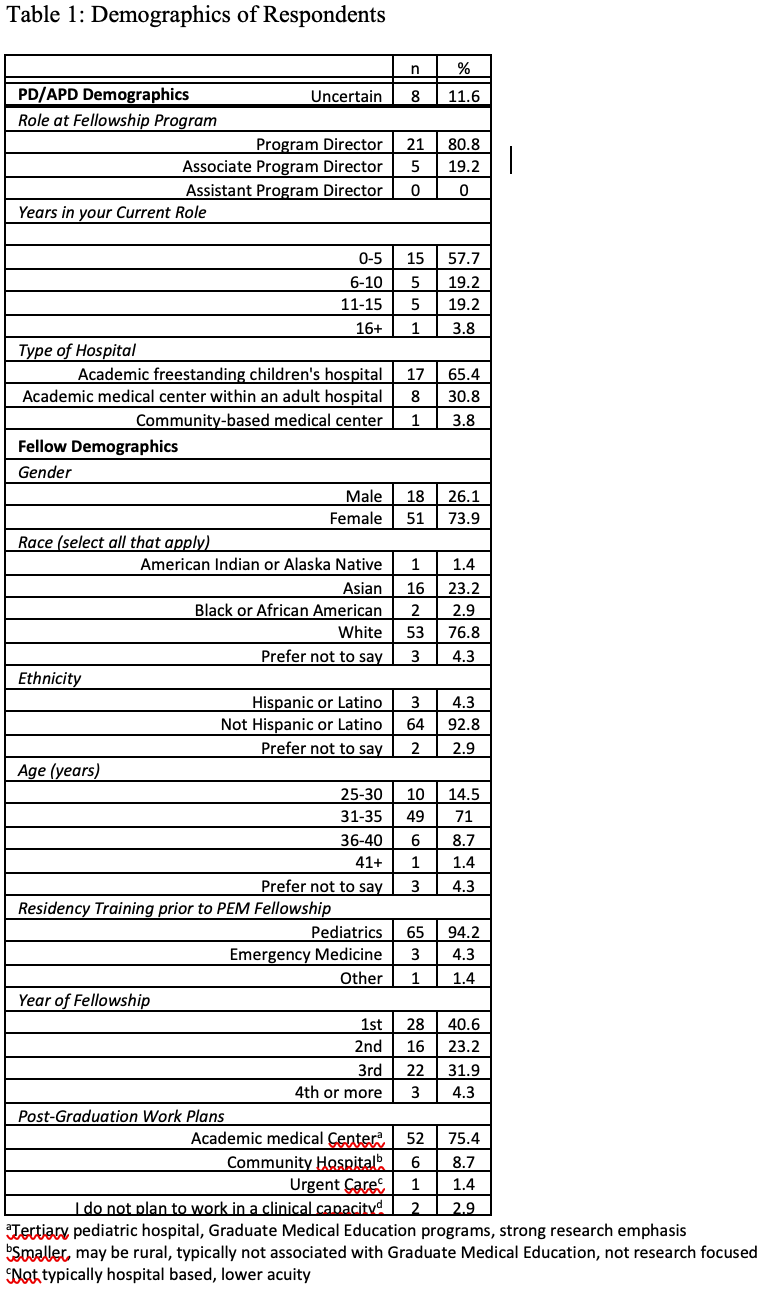
Design/Methods: In 2022, we developed and disseminated two separate electronic surveys to PEM program directors (PDs)/associate program directors (APDs) and PEM fellows through the American Academy of Pediatrics’ Section of Emergency Medicine PEM PD Survey Committee. The survey was open for five weeks and nonrespondents received three reminders.
Results: Over two-thirds of PDs/APDs (33%, n= 26/80) and 33% of PEM fellows (n= 69/211) completed the surveys. Of the respondents, 23% (n= 6/26) of PDs/APDs reported that their programs had a PEM fellow bedside teaching curriculum, while 40.6% (n= 28/69) of fellows reported that their programs had formal training in bedside teaching. Only 19.2% (n= 5/26) PDs/APDs, evaluated the effectiveness of their beside teaching curriculum. All PDs/APDs believed that their programs prepared fellows to be bedside teachers, while 82.1% (n= 55/67) of fellows agreed (p-value= 0.04). Most fellows (75.4%, n= 52/69) expressed interest in working at an academic medical center, of which 19.2% (n= 13/52) felt unprepared to be bedside teachers upon graduation. The majority of PDs/APDs (53.8%, n= 14/26), stated they were uncertain on how to create a bedside teaching curriculum. Most PDs/APDs (61.5%, n= 16/26) and fellows (60.9%, n= 42/69) noted that competing priorities and clinical expectations, respectively, were major barriers to learning bedside teaching.
Conclusion(s): With most PEM fellows likely working at an academic medical center upon graduation and most PEM programs not having a dedicated bedside teaching curriculum, there is a need for future studies to investigate how to encourage and implement bedside teaching education into PEM fellowship curricula.
.png)
.png)
