Mental Health
Mental Health 1
584 - Postpartum depression among newly delivered mothers based on neonatal disease severity in Lusaka, Zambia
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 584
Publication Number: 584.126
Publication Number: 584.126
Albert Manasyan, University of Alabama School of Medicine, Birmingham, AL, United States; Jyoti Lakhwani, University Teaching Hospital, Lusaka, Lusaka, Zambia; Herbert Kapesa, Center for Infectiouse Disease Research in Zambia, Lusaka, Lusaka, Zambia; Sylvia Machona, University Teaching Hospital, Lusaka, Lusaka, Zambia; Waldemar A. Carlo, University of Alabama School of Medicine, Birmingham, AL, United States; J. Anitha Menon, University of Zambia, Lusaka, Lusaka, Zambia

Colm P. Travers, MD
Assistant professor
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Postpartum Depression (PPD) is a serious public health problem affecting 17% of women globally, with higher rates recorded in Africa - 40%.
Objective: Our objective is to determine the prevalence of PPD among mothers based on the provided postnatal treatment for their newborn (Postnatal Ward, Neonatal Intensive Care Unit [NICU], and Kangaroo Mother Care ward [KMC]).
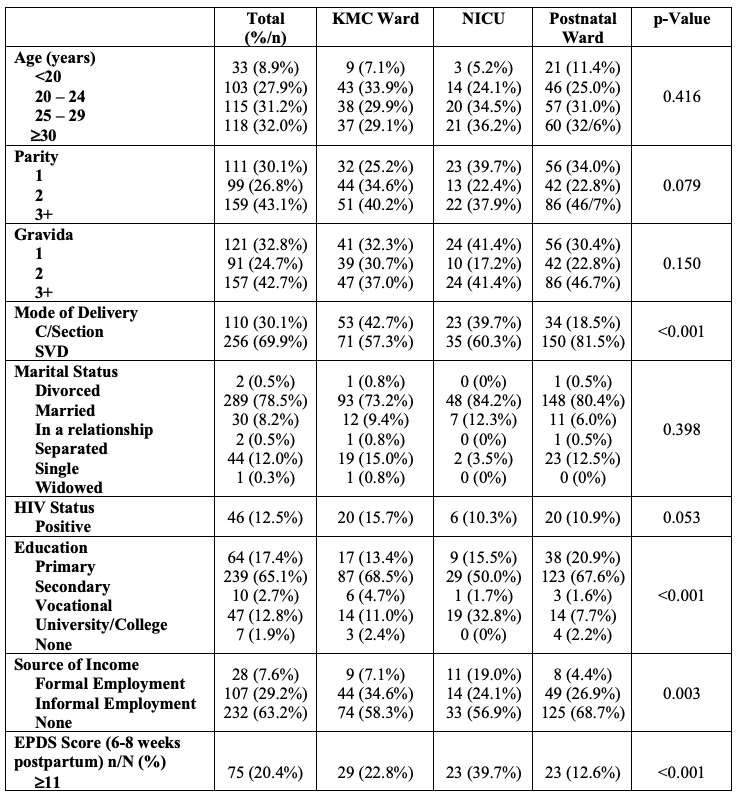
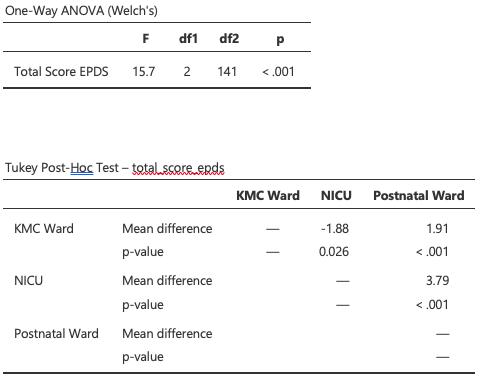
Design/Methods: We conducted a prospective study among newly delivered mothers at the Women and Newborn Hospital in Lusaka, Zambia between June and December 2022. Mothers of infants discharged home from the postnatal ward, KMC ward (admitted to the NICU then transferred to the KMC ward for step-down care before discharge home), and NICU (direct discharge home) were screened for PPD using the Edinburgh Postnatal Depression Scale (EPDS) screening tool at 6-8 weeks postnatally. Mothers who scored 11+ were categorized to have possible PPD. ANOVA was used to explore the difference in PPD in the study arms. The main outcome of interest was PPD following KMC, NICU, and postnatal ward discharge.
Results: We screened 369 newly delivered women for PPD pooled from mother-infant pairs admitted to the postnatal ward (n=184), KMC (n=127), and NICU (n=58). Overall, 65.1% of the mothers had secondary education, 63.2% were unemployed, 78.5% were married, and 12.5% were HIV-positive. Cesarean section rates were lowest among mothers in the postnatal ward (18.5%) and highest among those admitted to the KMC ward (42.7%). We recorded a negative correlation between birthweight and EPDS score (p=.005). While 20.4% of all mothers had PPD, mothers whose newborns were admitted to the KMC ward after NICU had a significantly lower rate of PPD (22.8%) compared to those directly discharged home from the NICU (39.7%) (p=.009). Most babies were admitted to the hospital for up to 5 days (52.3%).
Conclusion(s): While PPD screening is part of routine care in government health facilities in Zambia, it is not offered to pregnant or newly delivered women. KMC is associated with improvement in PPD among newly delivered mothers thus it should be considered for all mother-infant pairs discharged from the NICU. Furthermore, PPD screening should be offered during the postpartum period.