Medical Education: Resident
Medical Education 1: Resident 1
466 - Understanding Resident Note Writing Practices and Barriers: A Single Center Needs Assessment
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 466
Publication Number: 466.122
Publication Number: 466.122
Melissa N. Rodriguez Rodriguez, Emory University-Children's Healthcare of Atlanta, ATLANTA, GA, United States; Anjali Kirpalani, Emory University School of Medicine, Atlanta, GA, United States; Rebecca Sanders, Emory University/Children’s Healthcare of Atlanta, Atlanta, GA, United States; Sarah Varghese, Emory University School of Medicine/Children's Healthcare of Atlanta, Atlanta, GA, United States

Melissa N. Rodriguez Rodriguez, MD (she/her/hers)
PHM Fellow
Emory University-Children's Healthcare of Atlanta
ATLANTA, Georgia, United States
Presenting Author(s)
Background: Documentation can be time-consuming and may detract from patient care. Limited formalized curricula exist to educate pediatric residents on the development of requisite skills for effective and efficient note-writing.
Objective: To identify the educational needs of pediatric residents regarding efficient, and effective note-writing in the inpatient setting.
Design/Methods: Residents completed a survey to assess perceived barriers to note writing efficiency, impact on wellness, and insights on content for a future curriculum. We surveyed pediatric residents at a large academic center in February 2022 and new interns in September 2022.
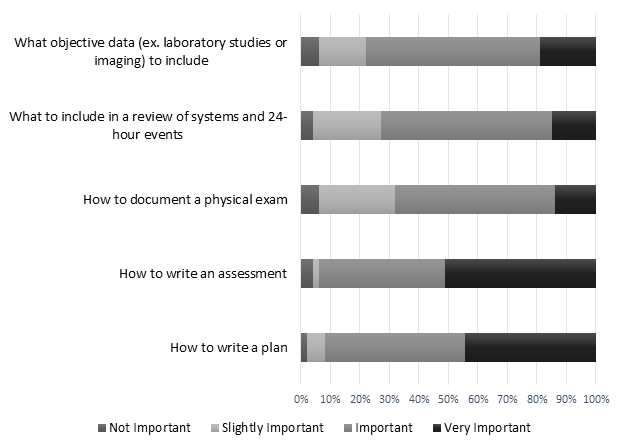
Results: 81/103 residents completed the needs assessment (combined response rate of 79%). 61% of participants rated billing as the most important reason to write a daily progress note, while only 3% rated communication among providers as the foremost reason. Third-year residents (PGY3s) reported greater comfort with writing a concise progress note for a hospitalized patient than first-year residents (PGY1s) [p=0.002]. PGY1s rated the assessment the most challenging part of note writing when compared to PGY3s [p=0.039]. PGY1s in February reported answering messages on a medical communication app to be an interference to note writing more frequently than PGY1s in September [p=0.024]. Patient care-related tasks, answering messages on medical communications apps, and completing admissions/discharges were common barriers identified by most residents (Figure 1). 74% reported note writing negatively impacts their well-being and 79% endorsed a negative impact on their joy at work. Open-ended questions revealed a desire for shorter rounding times and protected note-writing time. 75% of participants perceived formal feedback on progress notes from a supervisor would have been helpful at the beginning of residency. 42% of participants reported additional training on progress note writing in medical school would have been helpful. Instruction on how to write an assessment and plan were deemed to be the most important elements to include in educational programming on progress note writing (Figure 2).
Conclusion(s): Residents would benefit from additional educational training on the development of note-writing skills and best practices for efficiency at the beginning of or just prior to starting residency. This needs assessment led to the creation of a progress note curriculum for residents at our institution and inspired a quality improvement project aimed at streamlining the rounding process and protecting time for note writing.
.png)
