Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 1: GI Health and NEC Complications
340 - The Role of Epithelial and T Cell Dysregulation in Infants with Spontaneous Intestinal Perforation
Publication Number: 340.133

Abigail Jolteus (she/her/hers)
Undergraduate Research Assistant
Yale School of Medicine
Lake Park, Florida, United States
Presenting Author(s)
Background:
Spontaneous intestinal perforation (SIP) is a complication of prematurity that is characterized by a perforation in the terminal ileum and affects extremely low birth weight infants. Little is known about the etiology and pathogenesis of SIP. Preliminary data from our group suggests that defects in T cell population are evident at the time of SIP.
Objective:
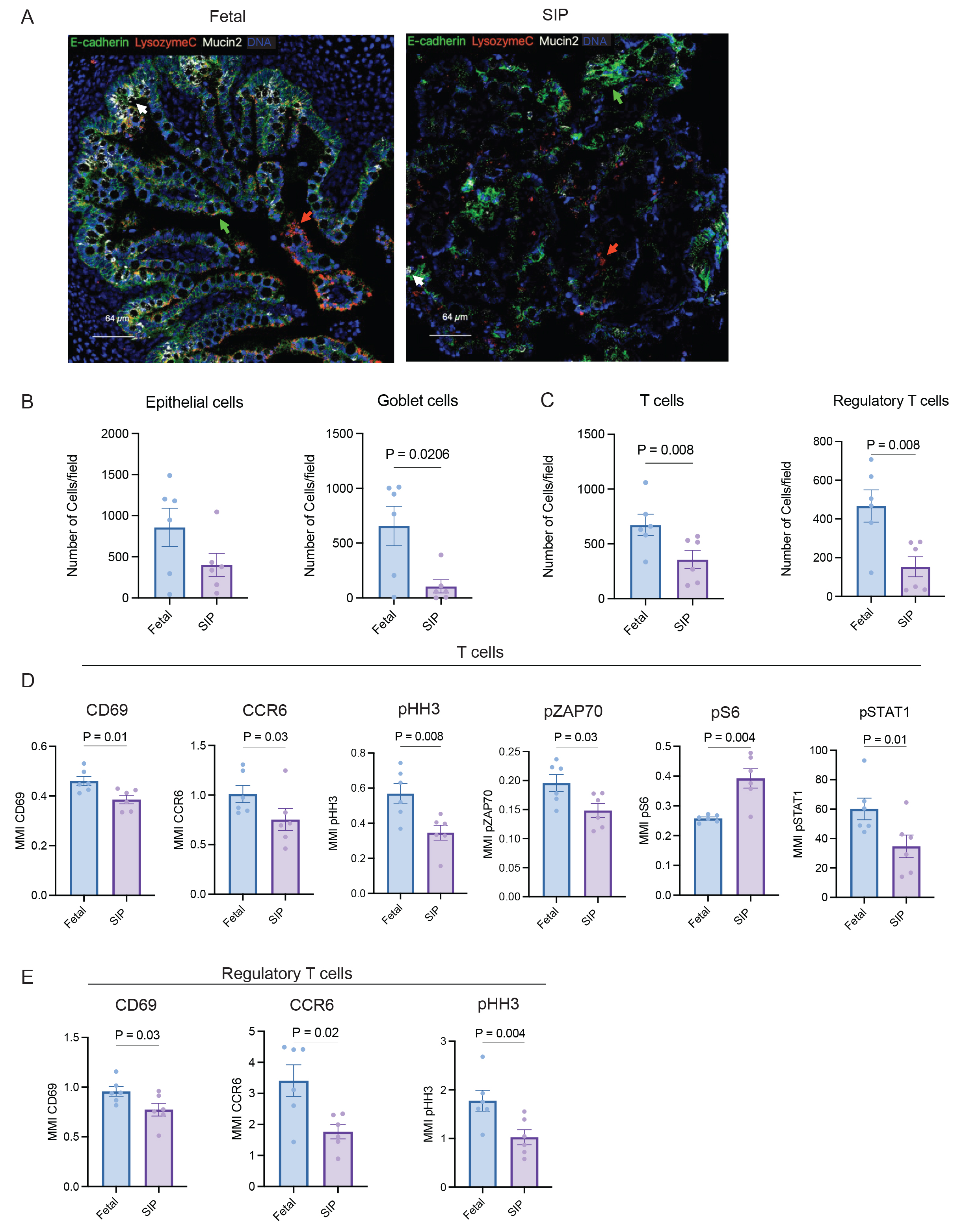
To determine the role of altered of T cells activation and epithelial cells function in SIP-affected mucosa using imaging mass cytometry (IMC). The epithelial barrier in SIP was structurally altered compared to fetal intestine (Fig 1A) with a marked decrease in goblet cells identified using mucin 2 (Fig 1B). There was a notable reduction in the total number of regulatory (Tregs) and total T cells in SIP compared to fetal intestinal mucosa (Fig 1C). The MMI expression of chemokine receptor (CCR6), type I interferon signaling (pSTAT1), proliferation (pHH3), activation (CD69) and TCR activity (pZAP70) was decreased on T cells in SIP compared to fetal samples (Fig 1 D, E). However, there was an increase in the expression of the mammalian target of rapamycin (mTOR) signaling/metabolism pS6 in SIP compared to fetal T cells (Fig 1D).
Design/Methods: Surgical samples from patients from Yale New Haven Children’s Hospital with SIP (n = 3; gestational age (GA) 23-26 weeks) were compared to small intestinal tissue from elective terminations (fetal n = 3; GA 21-23 weeks). Samples were formalin-fixed and paraffin-embedded and stained with a cocktail of 34 antibodies to identify epithelial, endothelial, fibroblast and immune cells using IMC. The abundance of major cell populations and median metal intensity (MMI) for activation markers and phosphoproteins were compared using a Mann-Whitney test.
Results:
Conclusion(s): In this study, SIP profoundly impacts the architecture of the epithelial barrier and the abundance and signaling of intestinal T cells. T cells in SIP show a reduction in markers of proliferation, migration, T cell receptor activation and type I interferon responses. The presence of altered T cell function is a potential mechanism for disease pathogenesis in SIP.