Neonatal Fetal Nutrition & Metabolism
Neonatal Fetal Nutrition & Metabolism 2: Neonatal Nutrition, Growth, and Outcomes
320 - Impact of a Nutritional Follow-up Program on Growth and Development in Premature Infants
Publication Number: 320.129
- SF
Sarah Fleishaker, MD (she/her/hers)
Fellow
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background:
Infants born premature are at higher risk of long-term growth and developmental delays, due in part to extra-uterine growth restriction (EUGR). Nutrition thus plays a large role in overall growth and neurodevelopment. Therefore, we created a special nutrition follow-up clinic for high risk preterm infants to monitor growth and assist with nutrition management.
Objective:
Primary objective was to evaluate growth of patients who attended a newly developed post-discharge nutrition clinic after discharge and to assess interventions performed. We also set out to compare growth parameters and developmental outcomes in the first year of life for preterm infants who attend a post-discharge nutrition clinic vs. those who do not,
Design/Methods:
Retrospective chart review of neonates born ≤ 32 weeks gestation and discharged home from the NYU Langone NICU. Subjects divided into 2 cohorts: One was subjects sent to a new post-discharge nutrition follow-up clinic and the other was a historical matched-control group of subjects discharged home prior to incorporation of this clinic. Exclusion criteria included those with congenital heart disease, abdominal surgery, a genetic syndrome diagnosis, or if no growth measurements existed in our system after discharge. Growth z-scores and Bayley scaled developmental scores were recorded. Data analysis performed using Student t-tests.
Results:
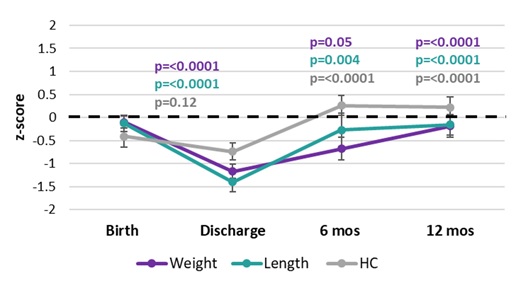
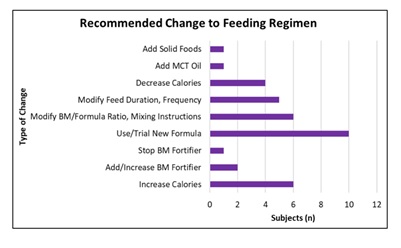
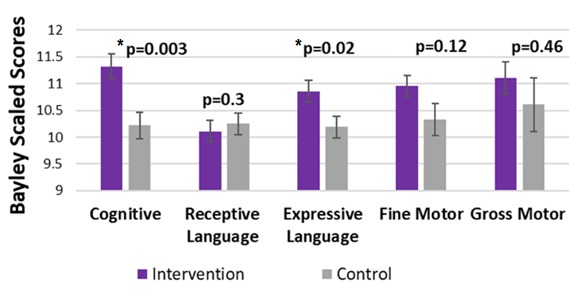
39 subjects in each group. There was significant improvement in all growth parameters for these EUGR infants who attended the new nutrition follow-up clinic from their discharge day to both 6 and 12 months after (see Figure 1). For these subjects, 36% had 1 follow-up visit, 28% had 2 visits, and 36% had ≥ 3 visits. A change to the feeding regimen was made at the initial visit 64% of the time. A variety of recommended changes to the nutrition plan occurred at clinic and are displayed in figure 2. When comparing growth between groups, no significant difference was observed in the first year after discharge. However, a difference in some developmental outcome scores was seen at 6 months after discharge (Figure 3) in subjects who attended nutrition follow-up clinic. This difference was no longer observed at 1 year post-discharge.
Conclusion(s): A nutrition follow-up clinic may be an important element for achieving favorable growth and developmental outcomes after NICU discharge. Optimizing nutrition quality, not just increasing caloric intake, may have an impact on development not reflected in standard growth measurements. Larger studies analyzing longer time points after discharge are needed.