Neonatal Neurology: Clinical Research
Neonatal Neurology 2: Clinical 2
167 - Association between continuous carbon dioxide monitoring and brain injury in infants receiving therapeutic hypothermia for neonatal encephalopathy
Publication Number: 167.136

Katie Hannon, BS (she/her/hers)
Research Assistant
Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Increasing evidence suggests that hypocapnia is associated with brain injury on MRI and adverse neurodevelopmental outcome in infants treated with therapeutic hypothermia (TH) for neonatal encephalopathy (NE). Consequently, continuous carbon dioxide (CO2) monitoring and avoiding extreme levels of CO2 have the potential to improve neurologic outcome.
Objective:
To compare changes in transcutaneous CO2 levels (tcPCO2) during hypothermia and rewarming between infants with and without brain injury on MRI in a cohort of infants with NE.
Design/Methods:
This prospective observational trial enrolled infants, who received TH for mild to severe NE between 2019 and 2022 at Brigham and Women’s Hospital. The tcPCO2 data was captured by a real-time integrated neuromonitoring system. We identified 2 groups of patients with and without any brain injury based on the assessment of MRI after rewarming. The median of tcPCO2 at each hour was calculated for each infant. Using these values, we calculated the mean tcPCO2 in each of seven phases of TH. The association between brain injury and tcPCO2 at each phase was analyzed using linear mixed models with fixed effects for group, phase, and their interaction and adjustment for correlation among repeated measurements. Differences between groups at each phase was determined using estimated marginal means.
Results:
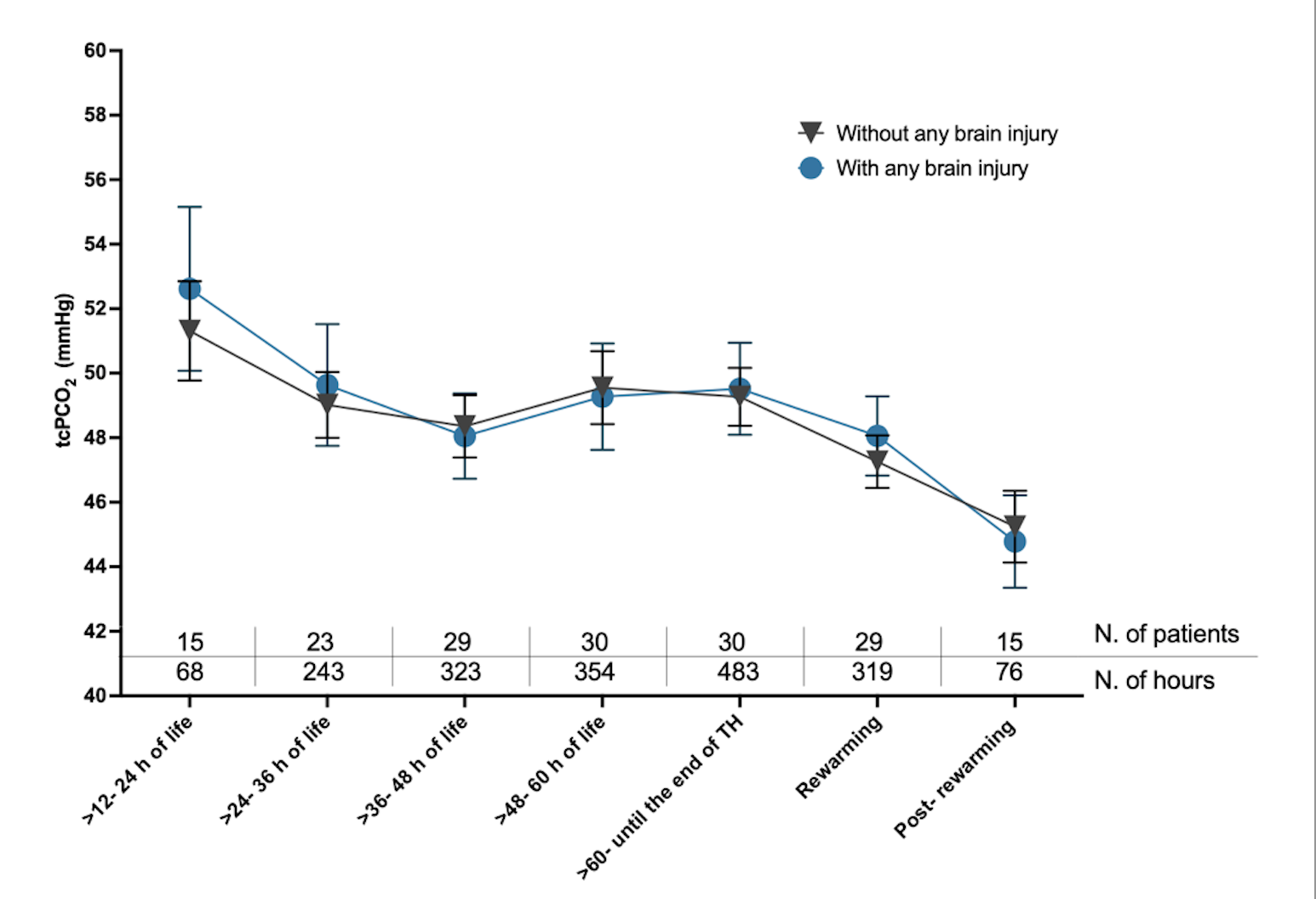
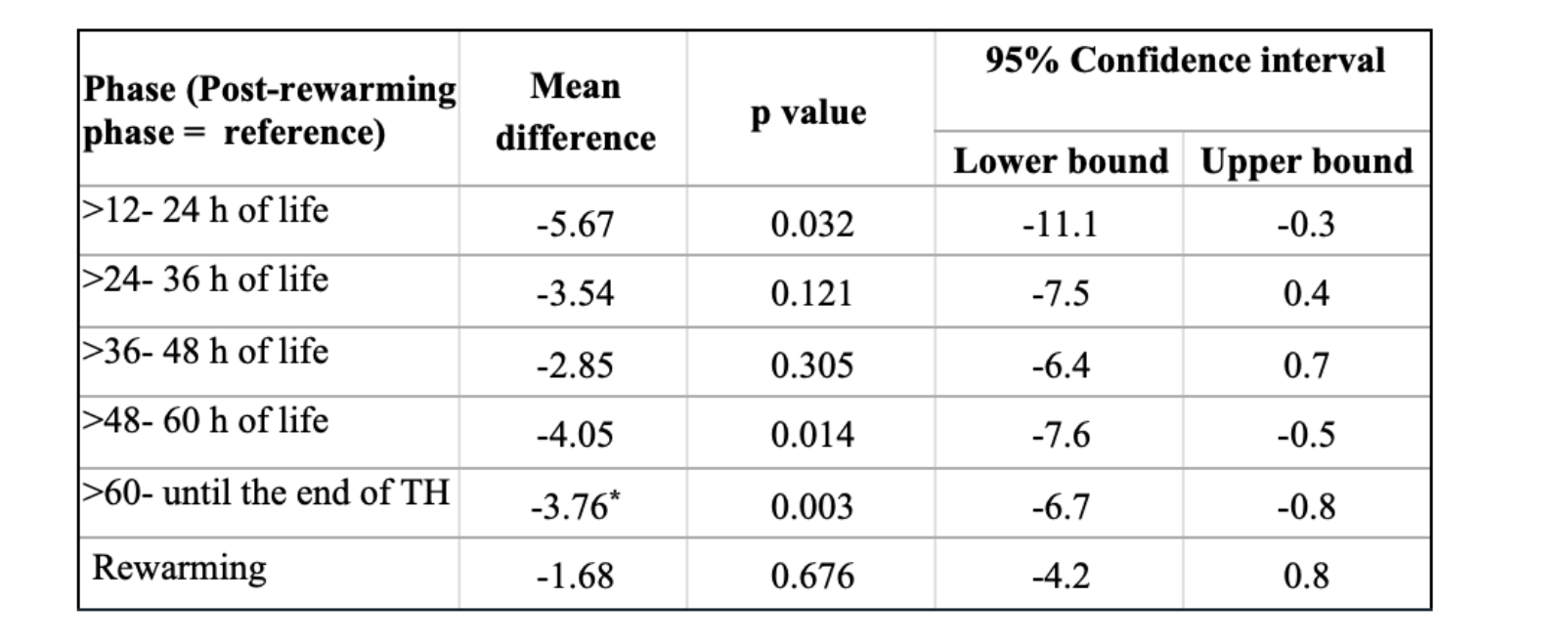
Serial measurements from 31 patients were available for analysis. Integrated monitoring began at median 24 hours of life (HOL, min-max: 11-51) and ended at median 94 HOL (min-max: 87-120). Sixteen (51.6%) infants had evidence of any brain injury on MRI. Results from mixed models indicated a significant effect of phase on mean tcPCO2 level (F =4.4, p= 0.001), but no difference by brain injury status (F= 0.0, p=0.304) or an interaction effect (F=1.2, p=0.304) (Figure 1). Mean levels of tcPCO2 exhibited a significant decrease between the last phase of TH (> 60 HOL) and post-rewarming phase. The pairwise comparisons between each phase and the post-rewarming period are summarized in Table 1.
Conclusion(s):
This novel longitudinal study of infants with NE across phases of TH showed relatively stable tcPCO2 levels within the normal range during hypothermia and rewarming but with a significant decline between the last phase of hypothermia and post-rewarming phase. The trajectories of tcPCO2 did not differ between infants with and without brain injury. These pilot results need to be interpreted with caution, increasing sample size and further investigations are needed.