Neonatal General
Neonatal General 2
272 - Neonatal Sequential Organ Failure Assessment Score as a Predictor of Length of Stay in the Neonatal Intensive Care Unit
Publication Number: 272.131

Devon Lewis (she/her/hers)
Medical Student
University of Chicago Division of the Biological Sciences The Pritzker School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background:
Preterm infants in the neonatal intensive care unit (NICU) are more likely to experience a long length of stay (LOS) in the hospital after birth. Factors used to predict LOS at birth may become less accurate depending on their clinical course. The neonatal sequential organ failure assessment (nSOFA) quantifies the severity of organ dysfunction in neonates throughout hospitalization.
Objective:
We aimed to measure the performance of nSOFA score for predicting LOS in a cohort of NICU patients.
Design/Methods:
We received expedited approval from University of Chicago IRB. The UChicago Medicine Comer Children’s Hospital has over 2400 deliveries per year. A retrospective chart review of the electronic medical record was completed on all infants admitted to the NICU at a single quaternary care site between 2009 and 2020. There were 8797 NICU admissions during the study period. Infants were excluded if they required transport to a higher-level facility, expired within admission, or were admitted to the general care nursery. Charts were interrogated for length of stay, birth weight, and components of nSOFA scores. Raw nSOFA scores were converted into categories. Category 1 was nSOFA scores 0-3, Category 2 scores 4-6, Category 3 scores 7-9, Category 4 scores 10-12, and Category 5 scores 13-15. Babies < 2.5 kg and >=2.5 kg were analyzed separately. Based on preliminary results, we chose our outcome as likelihood of LOS >90 days for < 2.5kg babies and >30 days for >=2.5 kg babies.
Categorical variables were compared using the Yates-corrected chi-squared test and continuous variables using the Mann-Whitney U test. Variables hypothesized to be associated with the outcome were first tested in univariate analysis using logistic regression. A multivariable logistic regression model was then used to evaluate the independent effect of significant clinical factors using backward selection. Data were analyzed using Stata version 14.
Results:
A total of 8534 NICU patients were included. There were 3700 patients with a birth weight < 2.5 kg. 479 (13%) had a LOS >=90 days. There were 4834 patients with a birth weight >=2.5 kg. 309 (6.4%) had a LOS >=30 days. Higher nSOFA score correlated significantly with greater odds of a LOS >90 days for babies < 2.5 kg (Table 2a) and LOS >30 days for >=2.5 kg babies (Table 2b). Higher nSOFA score was associated with a longer length of stay, whether the highest nSOFA score was within 1-24 hours, 3-24 hours, or 1-28 days (p< 0.001).
Conclusion(s):
After weight adjustment, the highest nSOFA score within 1-28 days is a good predictor of increased LOS for patients in the NICU.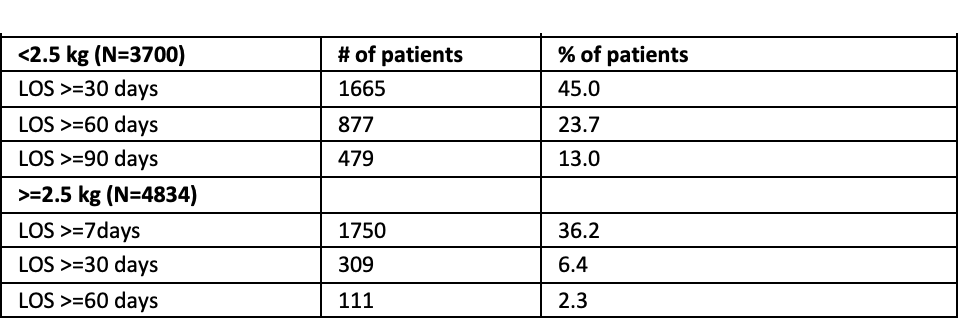
.png)
.png)
