Quality Improvement/Patient Safety: Improvement Science Research Methods
QI 1: Improvement Science Research Methods & Evaluation of QI Educational Interventions
677 - Impact of a digital sepsis recognition and management bundle at a children’s hospital: an embedded stepped wedge cluster design
Publication Number: 677.151

Warren M. Taylor, MD, MPH (he/him/his)
Pediatric Critical Care Medicine Fellow
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background:
Early recognition of possible pediatric sepsis, obtaining appropriate cultures, and treatment with antibiotics and fluids is associated with improved outcomes. Modern healthcare information systems may facilitate best practices and reduce infection-associated morbidity and mortality.
Objective: This study aimed to analyze the results of an inpatient sepsis guideline and order set were implemented at a large children’s hospital.
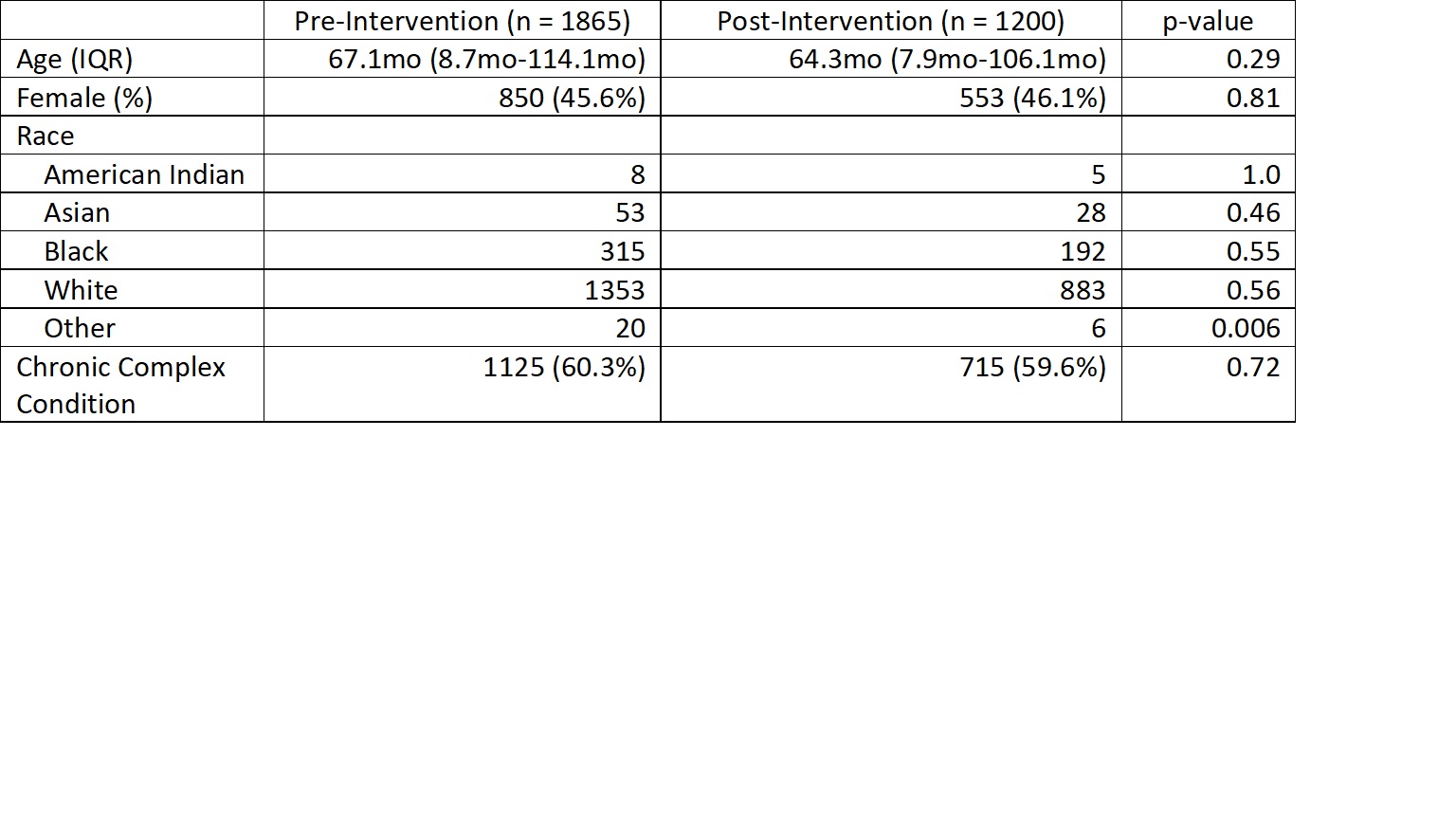
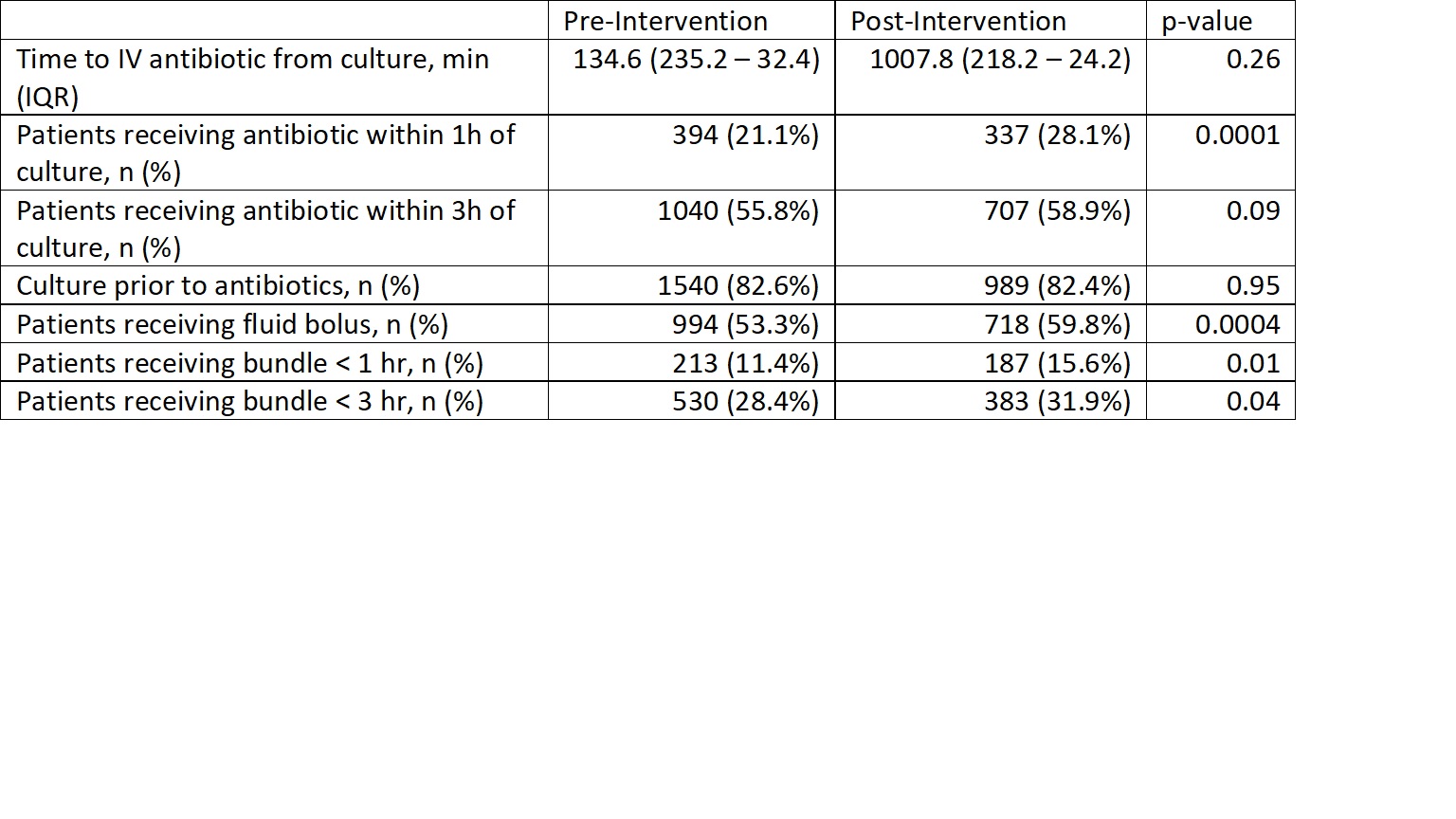
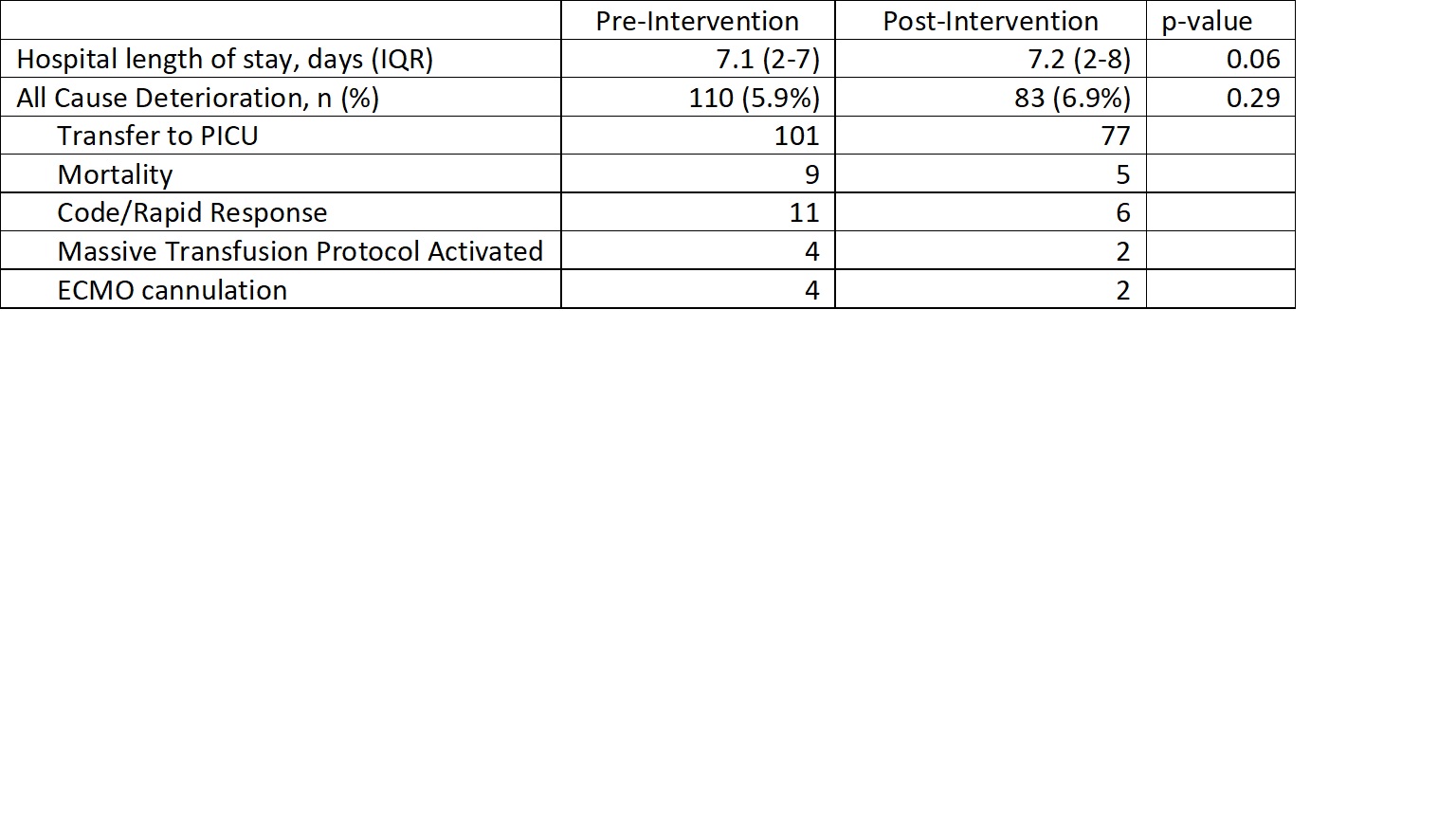
Design/Methods: Between January 2018 to April 2019, an electronic-record-integrated sepsis surveillance workflow was deployed with targeted education in a stepped wedge design across 8 inpatient, non-intensive-care unit (ICU) clusters. Tracking data, including outcomes, were encoded in informatics pipelines to facilitate performance assessments. Patients with possible sepsis, defined as receiving an intravenous antibiotic and body fluid culture, were included in a before-after analysis. Encounters with an associated ICD-10 code for sepsis were included in the stepped wedge analysis. Process measures included time to antibiotic and fluid bolus. Outcomes included length of stay (LOS), mortality, and all-cause deterioration. Chi-squared testing was performed for dichotomous variables, Mann-Whitney U for continuous variables, and logistic regression for multivariable models were conducted using R v4.1.2.
Results: There were 3065 patients with possible sepsis (1865 pre-, 1200 post-intervention) during the study period. Following guideline and treatment order set implementation, there was a significant improvement in patients receiving antibiotics within one hour of culture in the post vs pre-intervention period(337 [28.1%] vs 394 [21.1%]; P< 0.001), and a significant improvement in patients receiving antibiotics, a fluid bolus and having a culture obtained within both 1 hour (187 [15.6%] vs 213 [11.4%]; P=0.01), and 3 hours (383 [31.9%] vs 530 [28.4%]; P=0.04). One hundred twenty-six encounters had a sepsis diagnosis and a culture or antibiotic ordered outside of the ICU. In multivariable analysis accounting for the intervention and time among these patients, there was no significant association between LOS, mortality or all-cause deterioration and the intervention.
Conclusion(s):
After deployment of a digital sepsis recognition and management bundle at a large children’s hospital, there was a significant improvement in patients receiving antibiotics within 1 hour of cultures and in those receiving a culture, fluid bolus and antibiotic within 1 and 3 hours. A similarly designed electronic-record-integrated intervention could positively impact the care of children with sepsis.