Neonatal General
Neonatal General 2
270 - Examining the role of preeclampsia and chemokines on feto-placental stress
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 270
Publication Number: 270.131
Publication Number: 270.131
Sara Mohamed, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Niraj Vora, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Ram R Kalagiri, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Waverly B.. Waverly, Texas A&M Health Science Center College of Medicine, Temple, TX, United States; Muppala Raju, Baylor Scott and White Health/Texas A&M Health Science Center College of Medicine, Temple, TX, United States; Vinayak Govande, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Raza U Bajwa, Baylor Scott and White, Round Rock, TX, United States; Madhava R Beeram, Texas A&M Health Science Center College of Medicine, Temple, TX, United States; MOHAMMAD N N. UDDIN, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States

Sara Mohamed, MD (she/her/hers)
NICU Fellow
Baylor Scott White McLane Children's Medical Center
Temple, Texas, United States
Presenting Author(s)
Background: Preeclampsia (PreE) is the de novo development of hypertension and proteinuria after 20 weeks of gestation. It has a link to alterations of feto-placental stress that pass to the offspring causing detrimental effects.
Objective: To evaluate clinical outcomes and chemokines from maternal and cord blood in women with and without PreE.
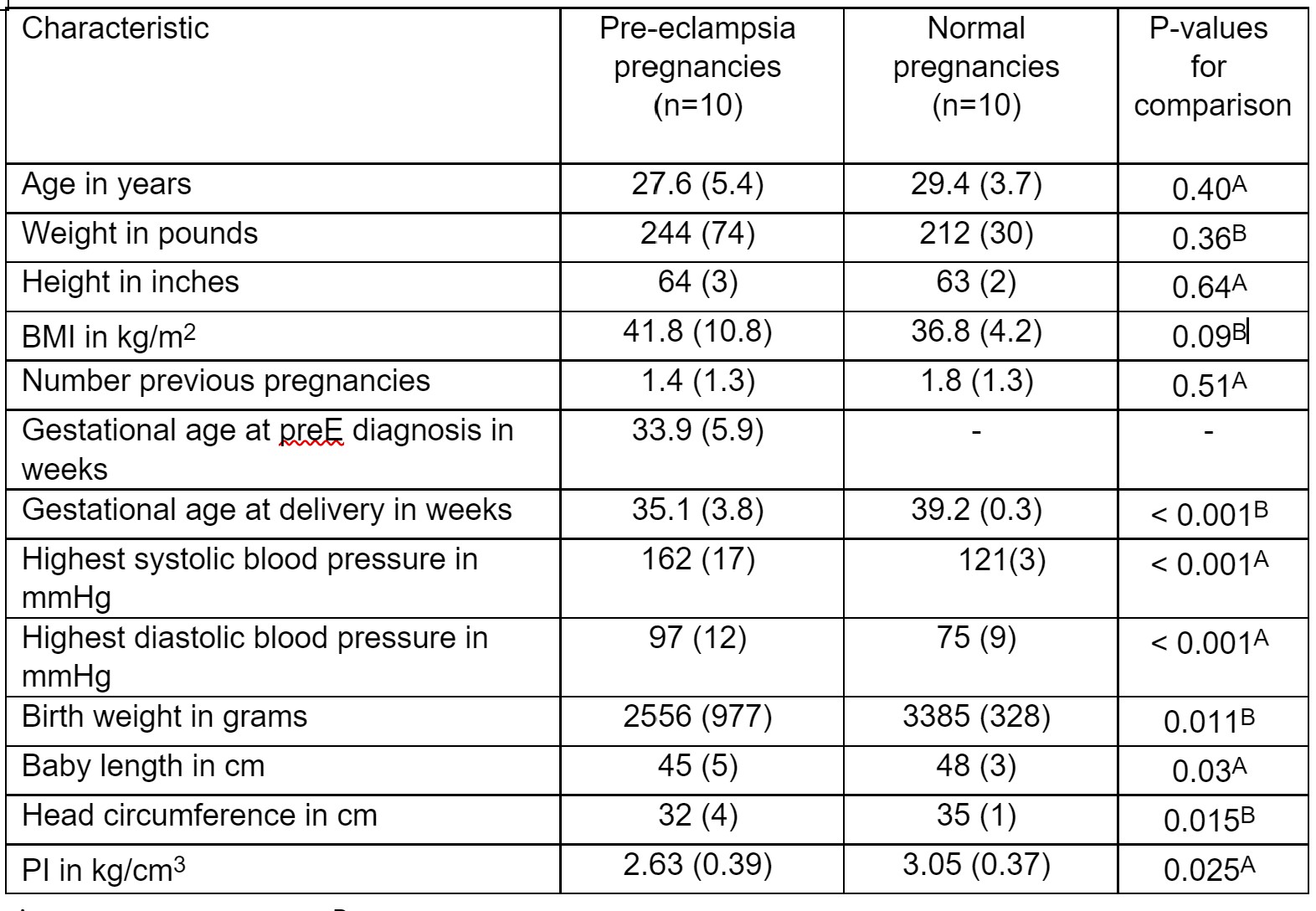
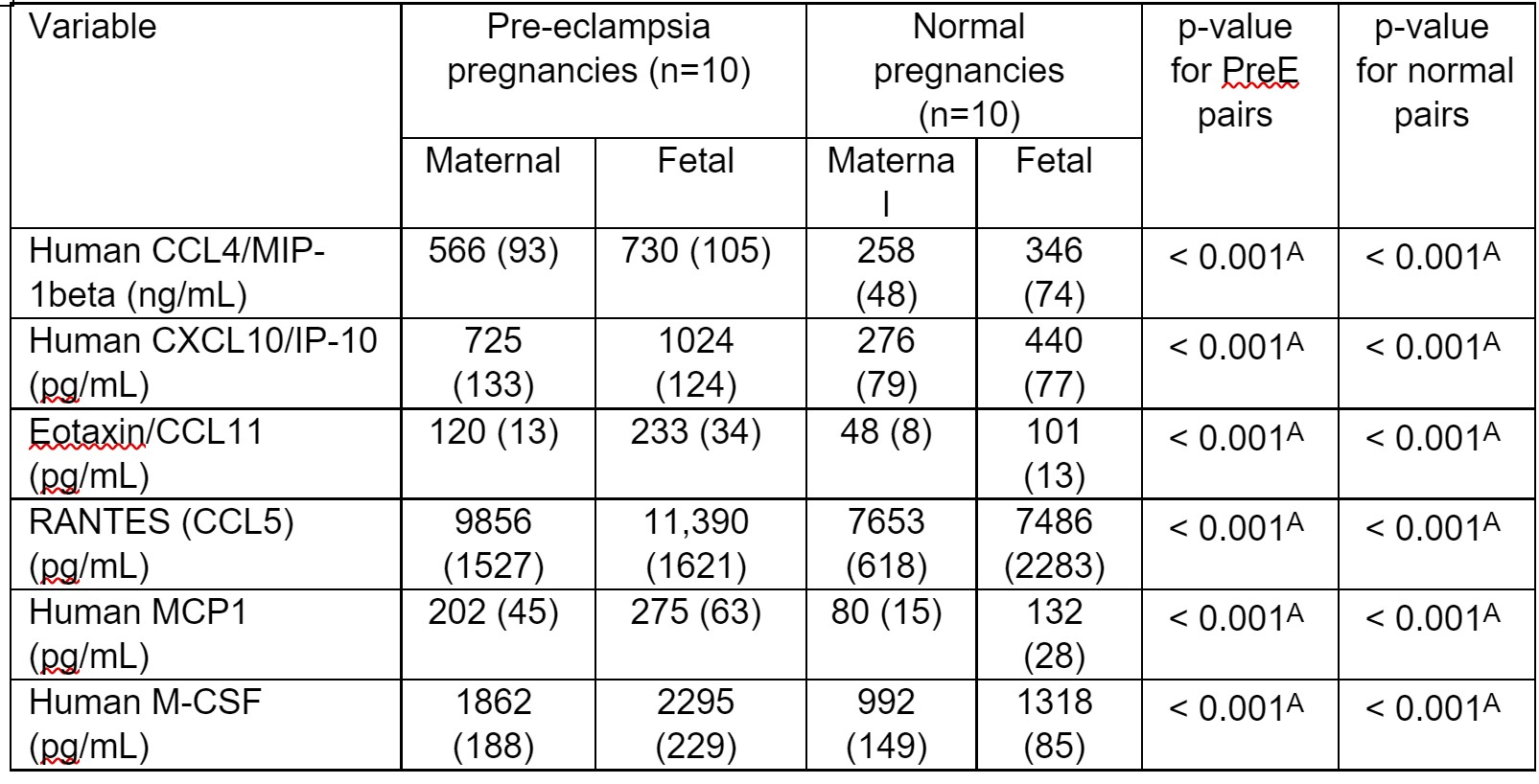
Design/Methods: Ten normal (NP) and Ten PreE pregnancies who delivered an infant at Scott & White Memorial hospital from November 2015 to November 2016 were recruited in a prospective cohort study. Serum levels of six chemokines in maternal-fetal paired samples were measured using commercially available ELISA. The markers are: Human CCL4/MIP-1beta, Human CXCL10/IP-10, Eotaxin/CCL11, RANTES (CCL5), Human MCP1, Human M-CSF. Chi square and paired t-tests were used to compare PreE patients to those with NP.
Results: Maternal systolic and diastolic blood pressure and maternal BMI were significantly higher in PreE women compared to NP. Infant gestational age and birth weight at delivery were lower in PreE compared to NP indicating a link to intrauterine growth restriction (IUGR). Maternal and fetal cord serum of six chemokines levels in mothers and their offspring differed in those with and without PreE (p< 0.001). A significant difference was detected between the maternal and fetal levels for the six chemokines (p< 0.01).
Conclusion(s): PreE increases the risk of fetal preterm deliveries and fetal IUGR. All six chemokines had significantly higher values in neonates compared to their mothers, which identifies the placental cell as the source, therefore, affirming the link between PreE and the altered intrauterine environment.