Quality Improvement/Patient Safety: Primary & Subspecialty Outpatient Quality Improvement
QI 2: Screening in Primary Care
687 - Standards of Care in Adolescent Preventative Medicine: QI Methodology to Improve Risk Identification and Provider Experience
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 687
Publication Number: 687.152
Publication Number: 687.152
William W. Sherrerd-Smith, Inova Children's Hospital, ARLINGTON, VA, United States; Paola Enid. Braña-Rivera, Inova LJ Murphy’s Children's Hospital, Fairfax, VA, United States; Courtney Port, Inova Children's Hospital, Falls Church, VA, United States; Albert V.. Brito, Inova Cares, Falls Church, VA, United States
.jpg)
William W. Sherrerd-Smith, MD (he/him/his)
Resident
Inova Children's Hospital
ARLINGTON, Virginia, United States
Presenting Author(s)
Background: Adolescent preventive healthcare can challenge providers to balance thoroughness, effectiveness, and efficiency. Risk-taking behaviors and mental health are the primary threats to morbidity and mortality in this age group, but discussing these topics can be complicated by social barriers and intrinsic features of adolescent development.
Objective: We aimed to improve preventative medicine encounters at our safety net clinic by providing a customized intake questionnaire alongside the Patient Health Questionnaire for Adolescents (PHQ-A), one-on-one time with providers, and discussion of confidentiality in >90% of annual well visits within the first three months of implementation. We aimed to accomplish this without reducing the detection of risk behaviors and without worsening provider experience.
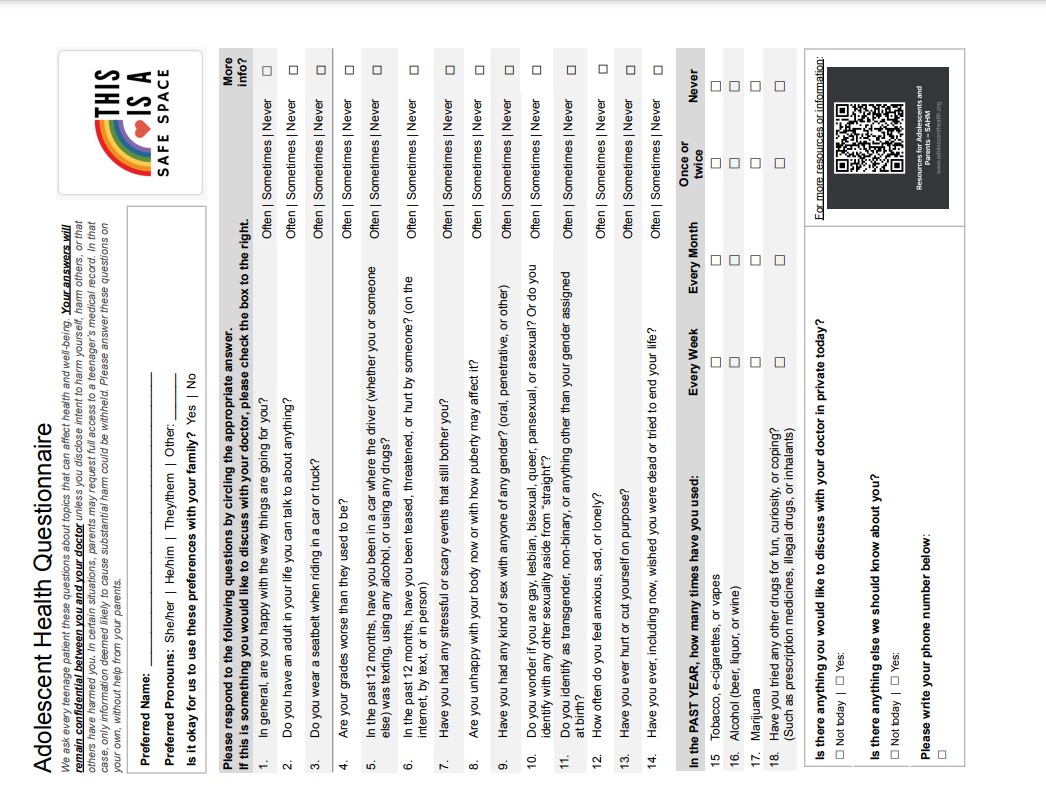
Design/Methods: The Model for Improvement was utilized in testing interventions through PDSA cycles. An intake questionnaire (figure 1) was adapted from the Minnesota AYA Health Questionnaire to help facilitate sensitive discussions. Sustainability interventions included provider education, streamlining the intake process, and adding note templates to serve as reminders. Deidentified response cards were completed by residents after every well visit for patients 12-17 years old. These cards asked for basic demographics, an assessment of risks based on clinical judgment, and simple feedback. This data was collected monthly and analyzed by the QI team on run charts.
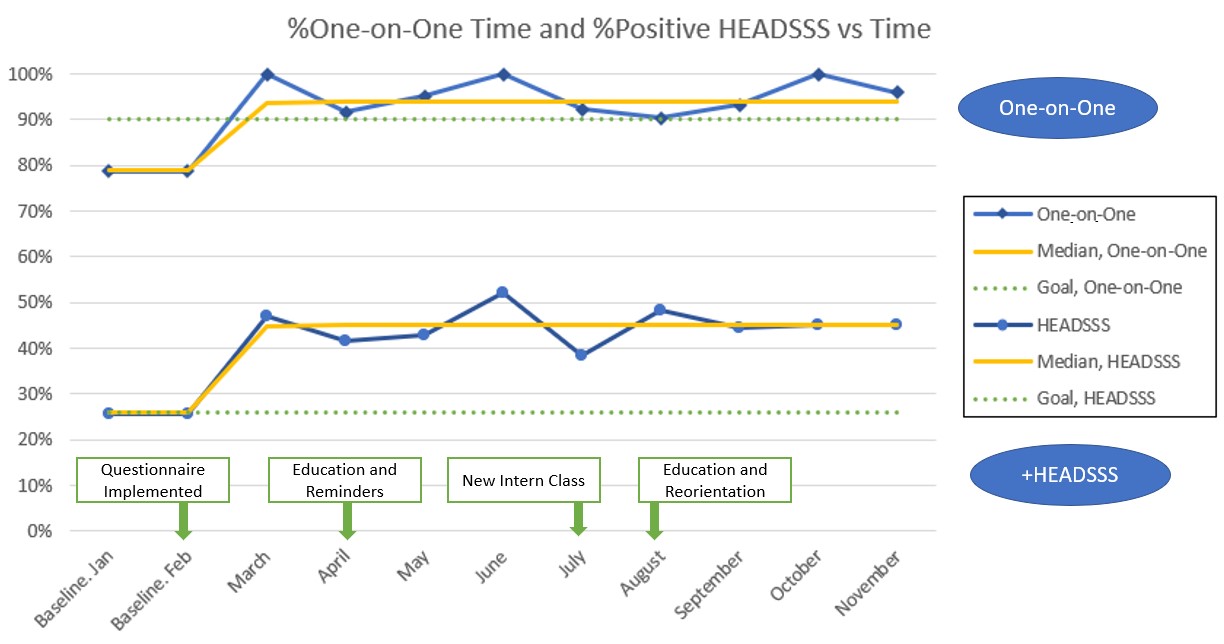
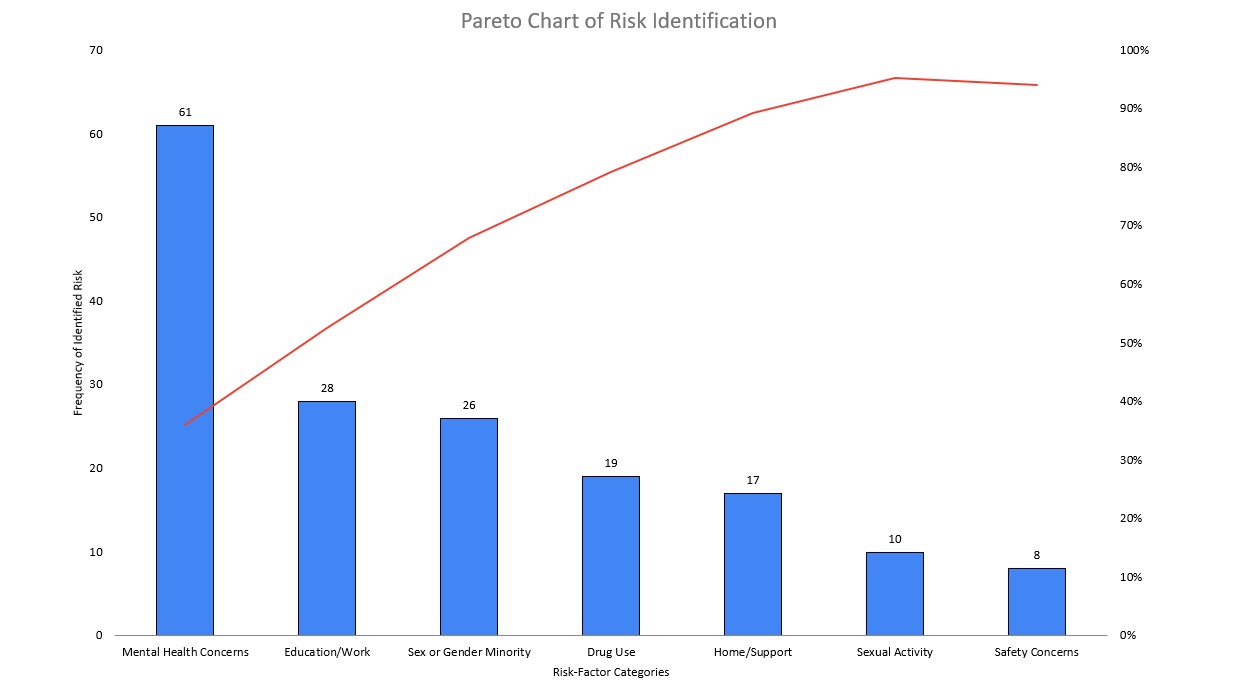
Results: Residents completed response cards in 70% (n=289) of qualifying adolescent well visits over 11 months. We increased confidentiality discussions from a median of 72% to 90% and the provision of one-on-one time from 79% to 94% (Figure 2). Identification of at least one risk-taking behavior increased from a median of 26% to 45%. Additionally, 35% (n=61) of the total findings were categorized as mental health concerns (Figure 3). Providers report that the questionnaire improved their workflow in 71% of visits. Only one visit was reported to be worse for it.
Conclusion(s): This project met its goals to standardize confidentiality discussions, one-on-one time, and distribution of the customized questionnaire and subsequently detected a higher rate of HEADSSS topics and improved provider experience. The shifts on the run chart coincided with the implementation of our surveillance questionnaire, but education, especially with new providers, was crucial to sustainability. In the future, we plan to streamline access to patient resources, especially with our high rate of mental health concerns.