Breastfeeding/Human Milk
Breastfeeding/Human Milk 2: Addressing Inequities in Lactation
377 - The Association between the Accumulation Effects of Early Life Human Milk Intake and Growth Outcomes in Very Preterm Infants
Publication Number: 377.102

Tsung-Yu Wu, Medical Doctor (he/him/his)
Attending physician
Ditmanson Medical Foundation Chia-Yi Christian Hospital
Chiayi City, Chiayi, Taiwan (Republic of China)
Presenting Author(s)
Background:
Human breast milk (HBM) is a crucial nutritional source for newborns, especially preterm infants. For the preemies unable to access their mother’s own milk (MOM), human milk bank provides an alternative source. Many recent studies have examined the composition difference between MOM and donor human milk (DHM), but the clinical impacts on preemies based on accumulation volumes are limited. We hypothesized that infants with greater MOM intake than DHM in early life would have better growth and lesser neonatal morbidities.
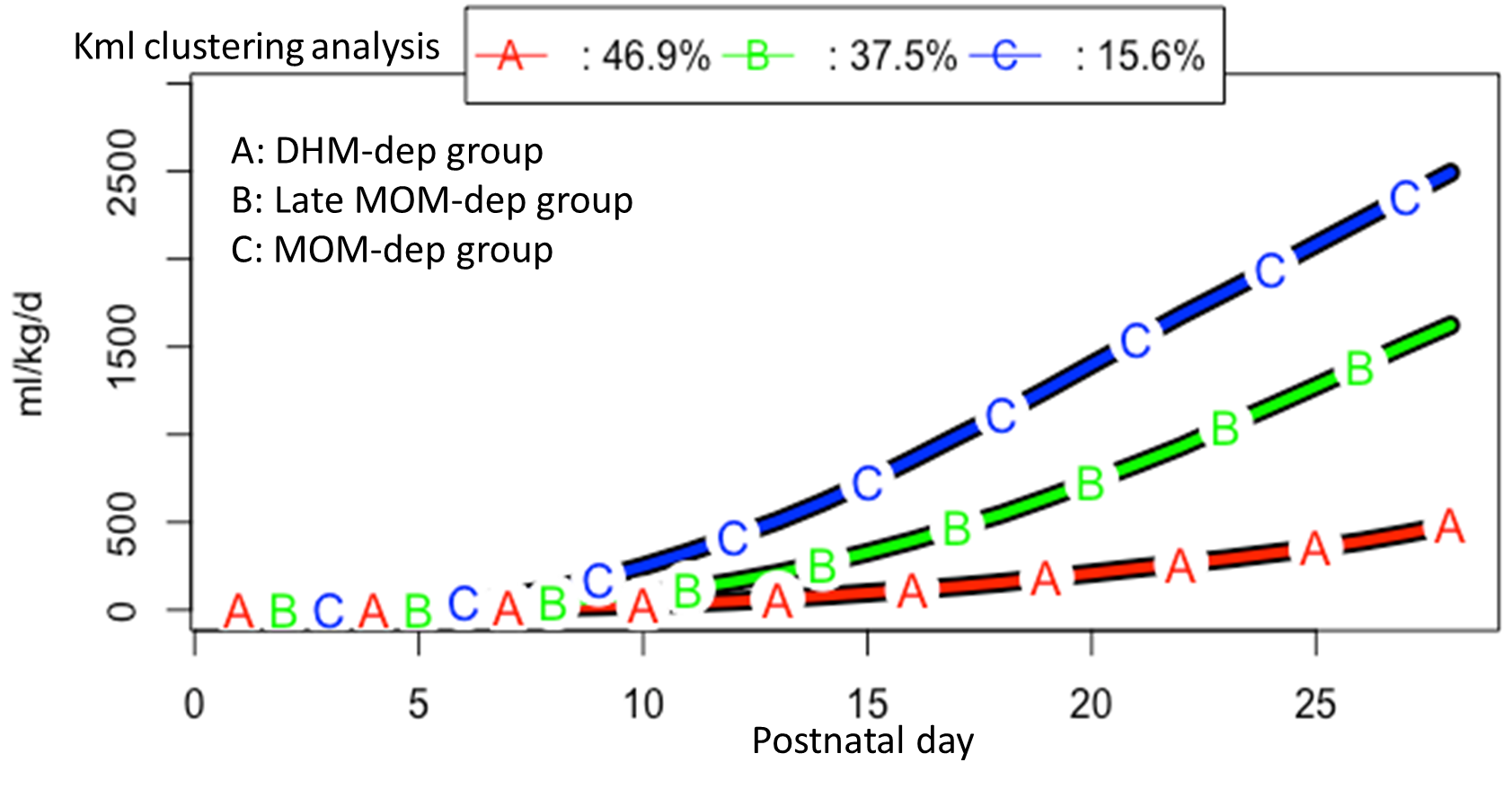
Objective: To establish different patterns of daily MOM utilization by K-means longitudinal (Kml) clustering analysis, and to compare the demographic data, major morbidities, and anthropometric outcomes between different patterns.
Design/Methods: This retrospective cohort study was conducted in a tertiary NICU at National Cheng Kung University Hospital in Tainan, Taiwan. We included very preterm infants (gestational age [GA] < 32 weeks) admitted within 3 days old from January 2015 to December 2016. Infants who had congenital anomalies or expired before discharge were excluded. The dependence of outcomes on the clinical variable was assessed by adjusting for priori covariates chosen to account for the clinical relevance and collinearity between variables and milk types. Kml clustering was applied to analyze daily intake in different milk types. Multivariable logistic regression analysis was performed to evaluate the crude effects of the potential independent variables.
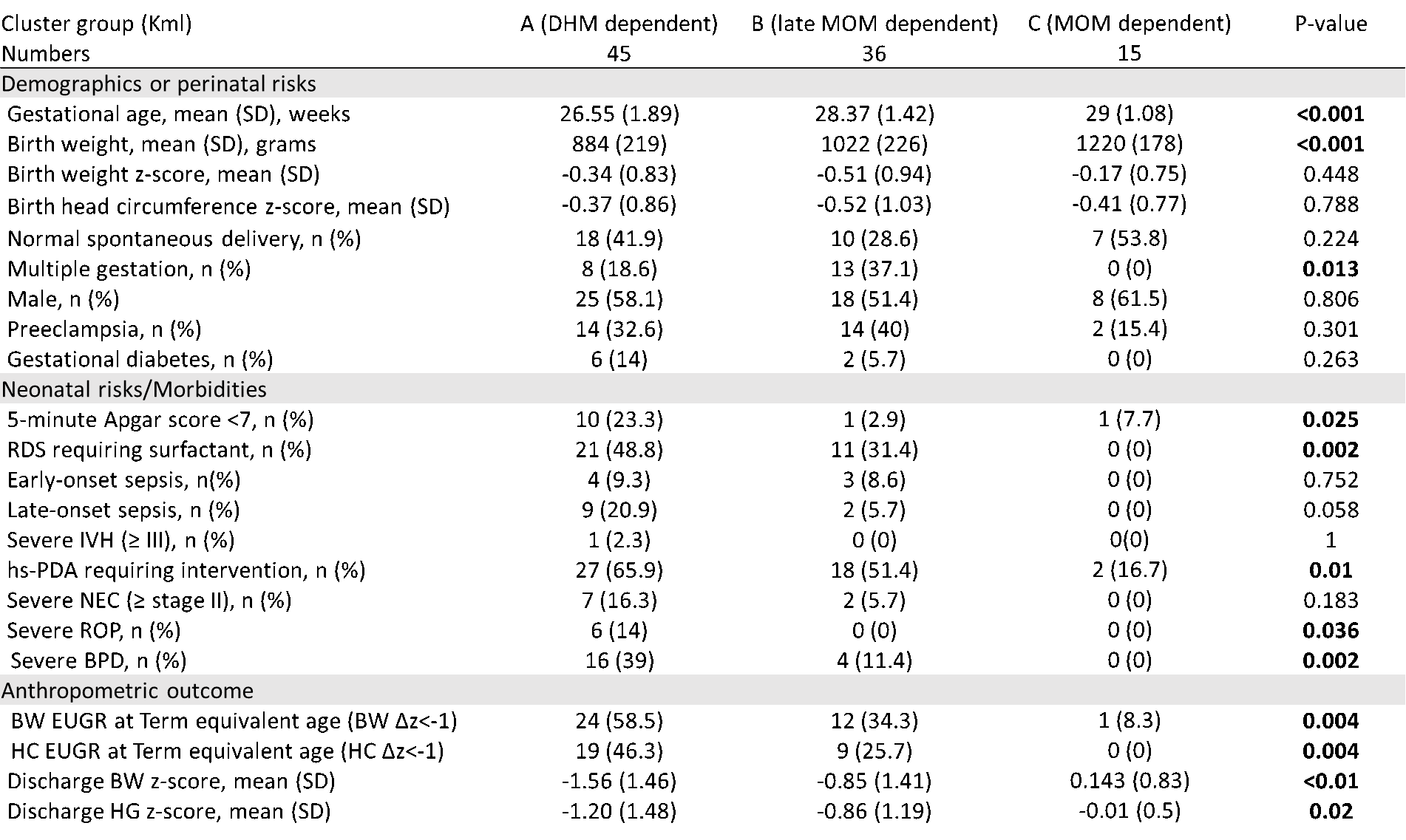
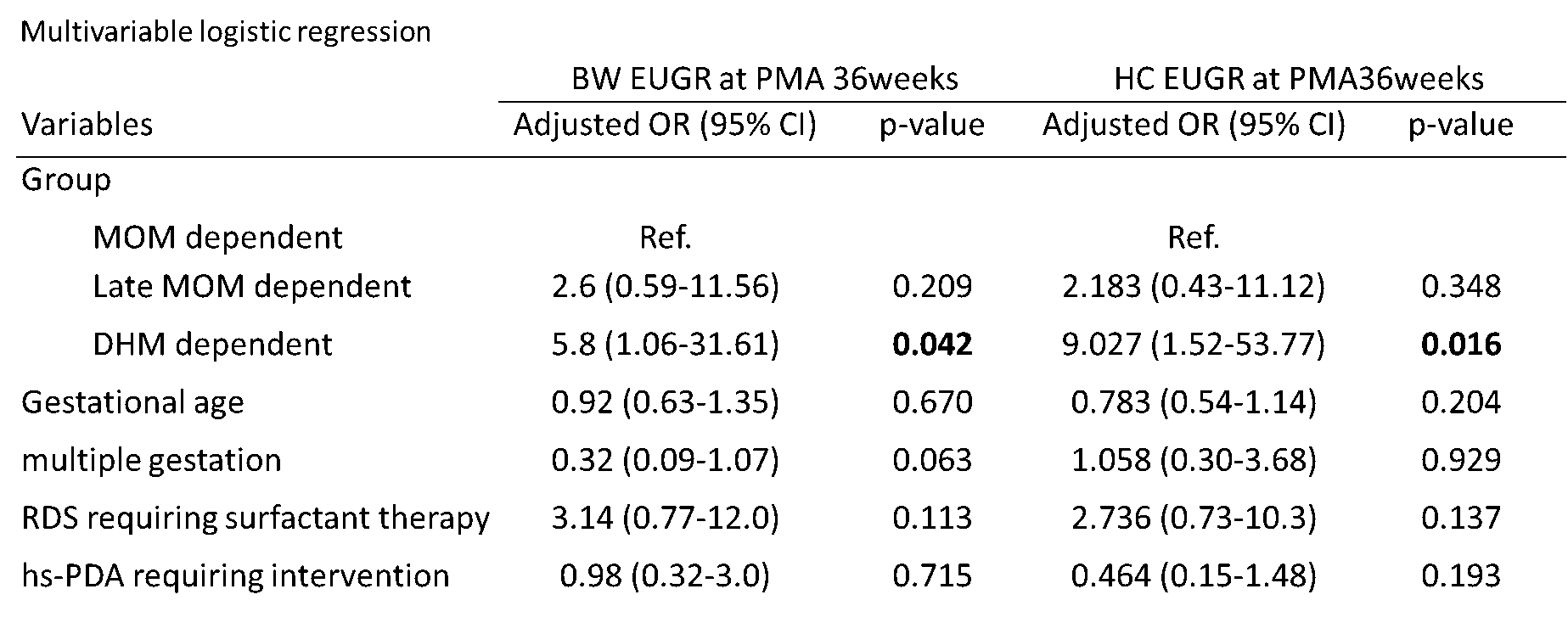
Results: The Kml clustering identified 3 distinct progression patterns (DHM-dependent [dep], late MOM-dep, MOM-dep) based on accumulation of daily MOM intake volume per kilogram for the first 28 postnatal days. Compared to the MOM-dep, the late MOM-dep and the DHM-dep groups were younger (GA: 29, 28.4, and 26.5 weeks, p< 0.001) and smaller (birth weight: 1220,1022 and 884 grams, p< 0.001). The DHM-dep group, compared to the MOM-dep group, had a significantly higher rate of extrauterine growth restriction at postmenstrual 36 weeks in body weight (BW) (58.5% vs. 8.3%, p=0.004; adjusted odd ratio [AOR]: 5.8, p=0.042), and in head circumference (HC). (46.3% vs.0%, p=0.004; AOR: 9.027, p=0.016)
Conclusion(s): Increasing early-life MOM intake may help in preterm growth in both BW and HC at postmenstrual 36 weeks. DHM-dependent preemies were at a higher risk of longitudinal head-size growth faltering, which was considered association with poor neurodevelopmental outcomes.