Neonatal Quality Improvement
Neonatal Quality Improvement 1
646 - Impact of a Bubble CPAP Protocol in Very Preterm Infants and Rates of Delivery Room Intubation, CPAP Failure and Death/Severe BPD – a 6-year Quality Improvement Study
Publication Number: 646.138
.jpg)
Gabriela de Carvalho Nunes, MD (she/her/hers)
Neonatologist
Saint John Regional Hospital, Horizon Health Network
Saint John, New Brunswick, Canada
Presenting Author(s)
Background: An interdisciplinary protocol using bubble continuous positive airway pressure (bCPAP) as first-line respiratory support in the delivery room (DR) and throughout hospitalization in the Neonatal Intensive Care Unit (NICU) was developed and implemented in 2014.
Objective: We aimed to evaluate the impact of this change on respiratory outcomes in preterm infants over time.
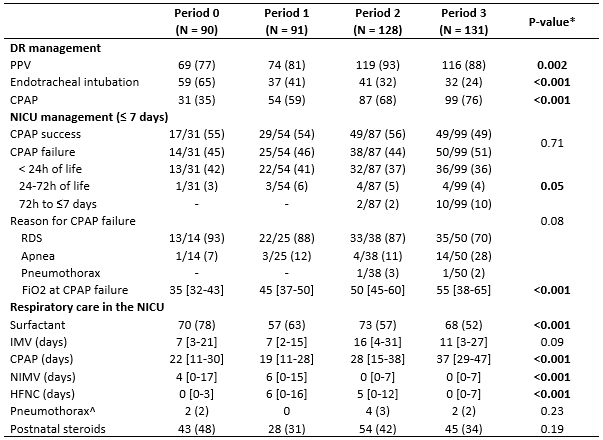
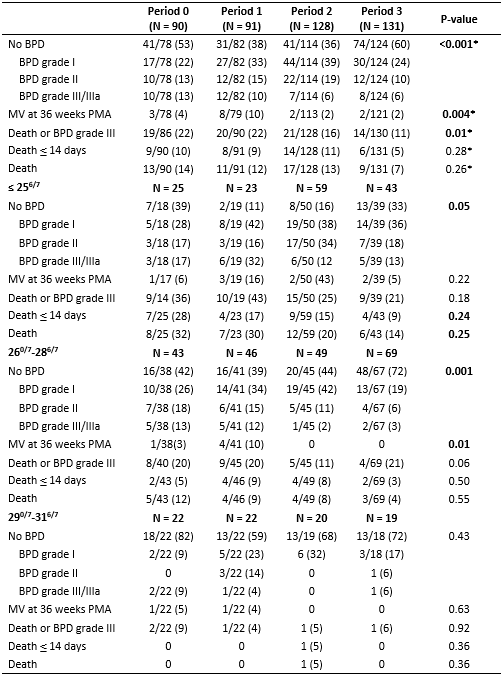
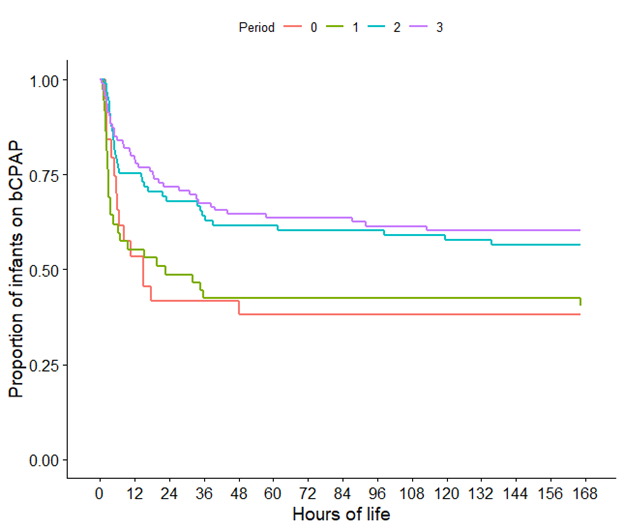
Design/Methods: Single centre cohort study including inborn infants without congenital anomalies born between 01/2012 and 06/2020 with gestational age < 32 weeks and birthweight < 1250g. To assess protocol impact over time, infants were grouped into periods: pre-implementation: 2012-2014 [P0], and post-implementation: 2014-2016 [P1], 2016-2018 [P2] and 2018-2020 [P3]. Outcomes were bCPAP in the DR, bCPAP failure ≤7 days of life (defined as endotracheal intubation), and death/severe BPD. The balancing measure was pneumothorax. Outcomes were compared between periods using logistic regression models adjusted for confounders. A Cox regression model was used to determine the association between periods and time to bCPAP failure.
Results:
A total of 440 infants were included (P0: 90, P1: 91, P2: 128, P3: 131). An increased proportion of infants < 26 weeks were admitted over time (P0: 76%, P3: 86%, p=0.006). The use of bCPAP in DR increased from 35% (P0) to 76% (P3) (Table 1, p< 0.001), most notably in infants born < 26 weeks (P0: 4% and P3: 60%, p< 0.001) and between 26-28 weeks (P0: 35%. P3: 80%, p< 0.001). Rates of bCPAP failure among infants not intubated in the DR were similar (P0: 45%, P3: 51%, p=0.71). NICU intubation occurred at higher O2 requirements (P0: 35% and P3: 55%, p< 0.001) and at later chronological age, with the lowest odds of intubation in P3 (Figure 1, Hazard ratio 0.44, 95% CI 0.23-0.86, p=0.01). A trend towards less exposure to postnatal steroids was noted (P0: 48%, P3: 34%, p=0.19). Six years after protocol implementation, more infants were free of BPD (P0: 53%, P3: 60%, p< 0.001), and the proportion of severe BPD decreased (P0: 13%, P3: 6%, p< 0.001), which was mainly driven by infants born < 29 weeks (Table 2). Overall death/severe BPD rates significantly decreased from 22% (P0) to 11% (P3), even after adjusting for possible confounders. Death rates were similar (P0: 14%, P3: 7%, p=0.26).
Conclusion(s): In extremely preterm infants, implementing a comprehensive bCPAP protocol starting in the DR and extending throughout hospitalization significantly improved respiratory outcomes over time, despite treating smaller and more immature patients.