Quality Improvement/Patient Safety: Primary & Subspecialty Outpatient Quality Improvement
QI 2: Screening in Primary Care
686 - Improving STI Screening in Adolescent and Young Adult Males
Publication Number: 686.152
- JA
Jessica Addison, MS,MS,MPH (she/her/hers)
Faculty
Boston Children's Hospital, Division of Adolescent/Young Adult Medicine
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Adolescents and young adults (AYAs) account for approximately half of all new diagnoses of sexually transmitted infections (STIs) in the United States. Screening AYA males is imperative to stopping the spread of infection as well as long-term sequelae. While our AYA medical practice has consistently screened AYA females at rates above 80% annually for years, the baseline screening for males is less than 70%. Notably, AYA males had unique barriers to screening and limited testing options during the COVID-19 pandemic (i.e., limited urine testing due to supply chain issues).
Objective:
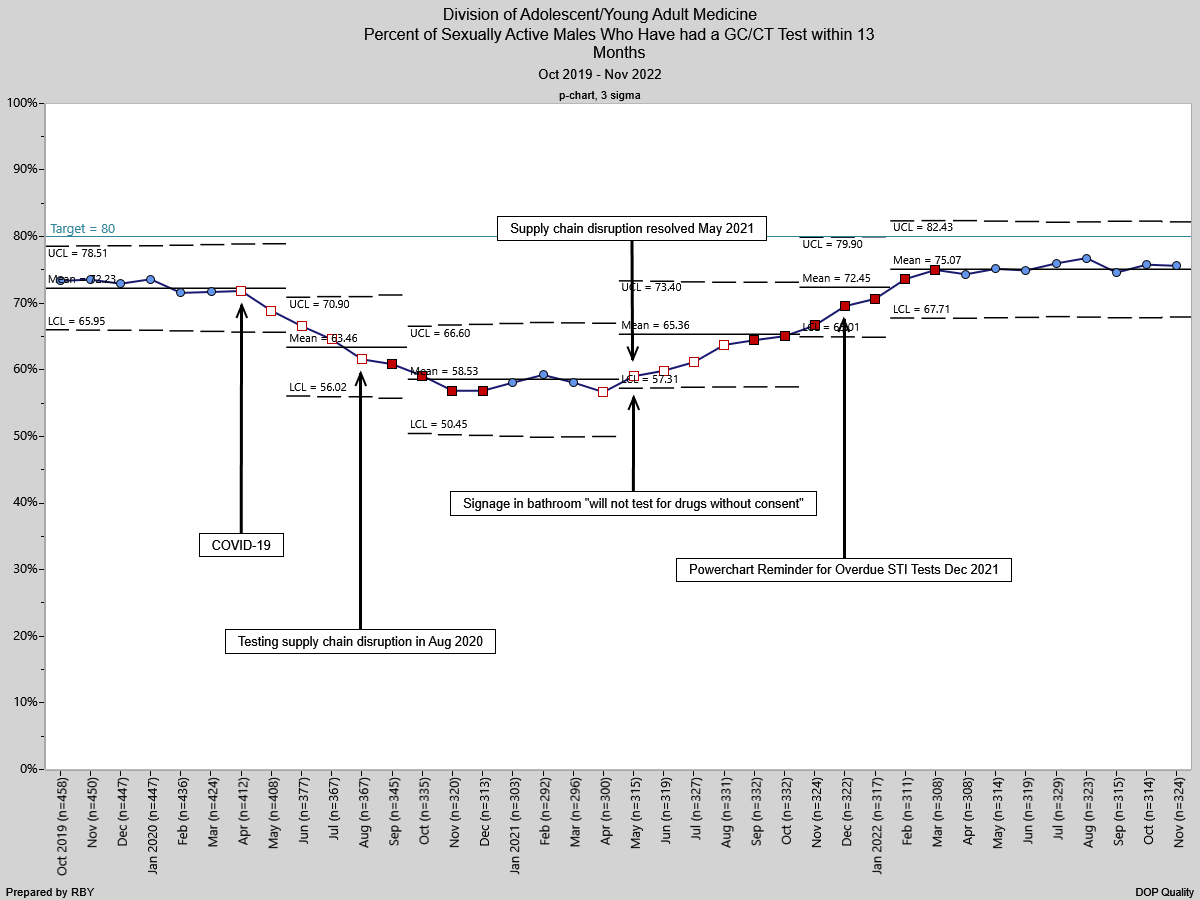
Increase Gonorrhea/Chlamydia (GC/CT) screening in AYA males with in-person visits from the nadir level of 58% during the pandemic to 80% (above pre-COVID high) by July 2022.
Design/Methods:
Development of a process map, fishbone diagram, and driver diagram were used to assess core issues and consider interventions. Multiple Plan, Do, Study, Act (PDSA) cycles have been implemented. The first PSDA cycle included adding a bathroom sign clearly stating urine would not be tested without patient’s consent to address concerns regarding drug testing. The second PDSA cycle involved creation and implementation of a testing alert for all male medical visits. Our electronic health record (EHR) was used to generate a weekly list of patients with upcoming visits who last had GC/CT testing greater than 13 months prior, and thus overdue for annual screening. A note was added to “reason for visit” within a patient’s chart indicating they were overdue for STI testing. This prompted clinical assistants to provide a urine cup and prompted clinicians to discuss STI testing. A p-chart was used to compare baseline to post-intervention period testing rates. This study was reviewed by Boston Children’s Hospital Quality Improvement (QI) Committee and considered IRB exempt.
Results:
Statistical Process Control p-chart analysis showed special cause variation with a significant increase in the mean screening rate from 58% to 65% with initiation of our first intervention. Following our second intervention rates increased to over 75%, demonstrating a mean shift from previous results. The p-chart demonstrates a trend toward improving screening rates following our PDSA cycles but remains under our target goal of 80%.
Conclusion(s):
The following interventions have improved GC/CT screening rates among AYA males: bathroom signage indicating patient’s consent prior to testing and EHR prompt for clinic staff regarding overdue STI testing. A future initiative includes creating an automated reminder within the EHR for all AYA patients with overdue STI screening.