Neonatal General
Neonatal General 3: Ethics, Parents Take the Lead
285 - The Moderately Preterm Infant Parent NICU Experience: Opportunities for Improvement
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 285
Publication Number: 285.132
Publication Number: 285.132
Ashley D. Osborne, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Diana Worsley, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Catherine E. Cullen, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Lori Christ, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Ashley D. Osborne, MD (she/her/hers)
Fellow Physician
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Many parents of preterm infants feel stressed and unprepared for discharge from the neonatal intensive care unit (NICU). Although moderately preterm infants (MPTI) experience fewer complications of prematurity than infants born at lower gestational ages, they comprise a large proportion of NICU admissions and often require hospitalization for weeks. Learning more about the MPTI birth parent experience can inform targeted interventions to improve family centered care and outcomes for this population.
Objective: Describe knowledge gaps, discharge readiness and communication preferences of parents of MPTIs to inform future design of interventions
Design/Methods: Semi-structured qualitative interviews were performed with English-speaking birth parents of infants born between 32-34 weeks gestation at the Hospital of University of Pennsylvania Level III NICU. Interviews were performed at a mean of 32 ± 14 days post-discharge via phone and lasted 25-45 minutes. Two team members analyzed the recorded, transcribed interviews using a modified grounded theory approach. Enrollment ceased when the data reached thematic saturation. NVivo 12 facilitated the data analysis.
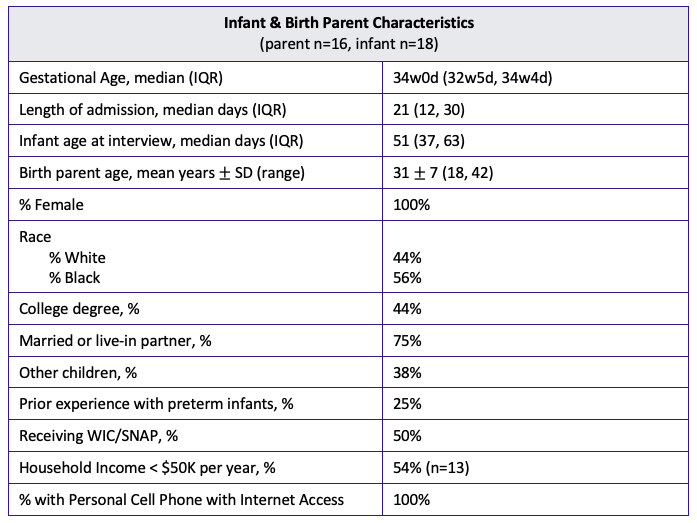
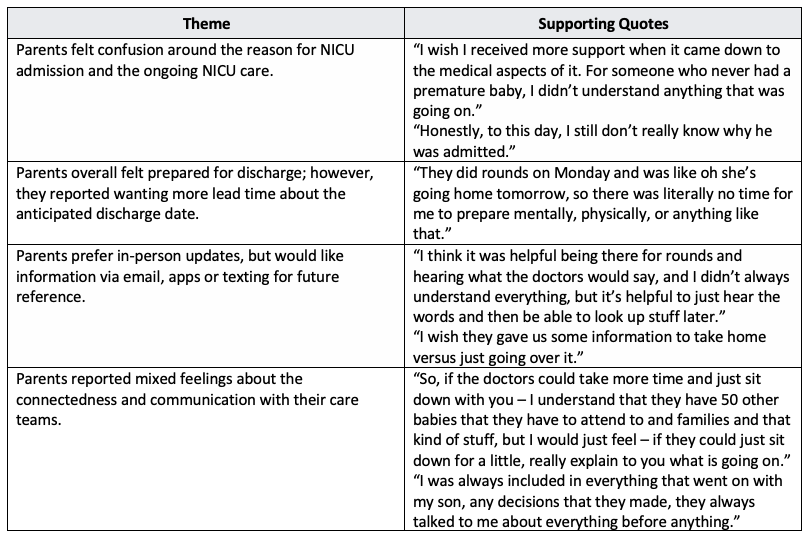
Results: Thematic saturation was reached after 16 parent interviews. Table 1 shows infant and parent characteristics. Parents described the NICU admission as being stressful and overwhelming. Four major themes emerged surrounding parent confusion, the discharge process, the perceived benefits of electronic health resources, and parent-medical team connectedness (Table 2). Some respondents felt they did not receive the important information they needed to care for their preterm infant at home, while others felt very informed. Additionally, parents desired more education regarding feeding, reflux, breathing patterns, and routine infant care around discharge.
Conclusion(s): Parents of MPTIs describe the NICU experience as stressful, despite this population’s relatively lower rate of prematurity complications. They report valuing a strong connection with the medical team with good communication and shared decision making. They also described gaps of knowledge regarding reasons for admission and ongoing management, desiring more advanced notice of discharge, and the potential benefit of electronic resources. These results serve as a foundation for future quality improvement projects, including the development of a texting-based virtual assistant in our unit to improve parental understanding of the implications of prematurity, discharge readiness and emotional well-being of MPTI parents.