Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 1: Epi/HSR Equity
616 - Lactation Experiences of Black Mothers of Infants in the Neonatal Intensive Care Unit
Publication Number: 616.14

Alissandre T. Eugene, Bachelor's of Science (she/her/hers)
Undergraduate Research Assistant
University of Florida College of Medicine
Ocala, Florida, United States
Presenting Author(s)
Background:
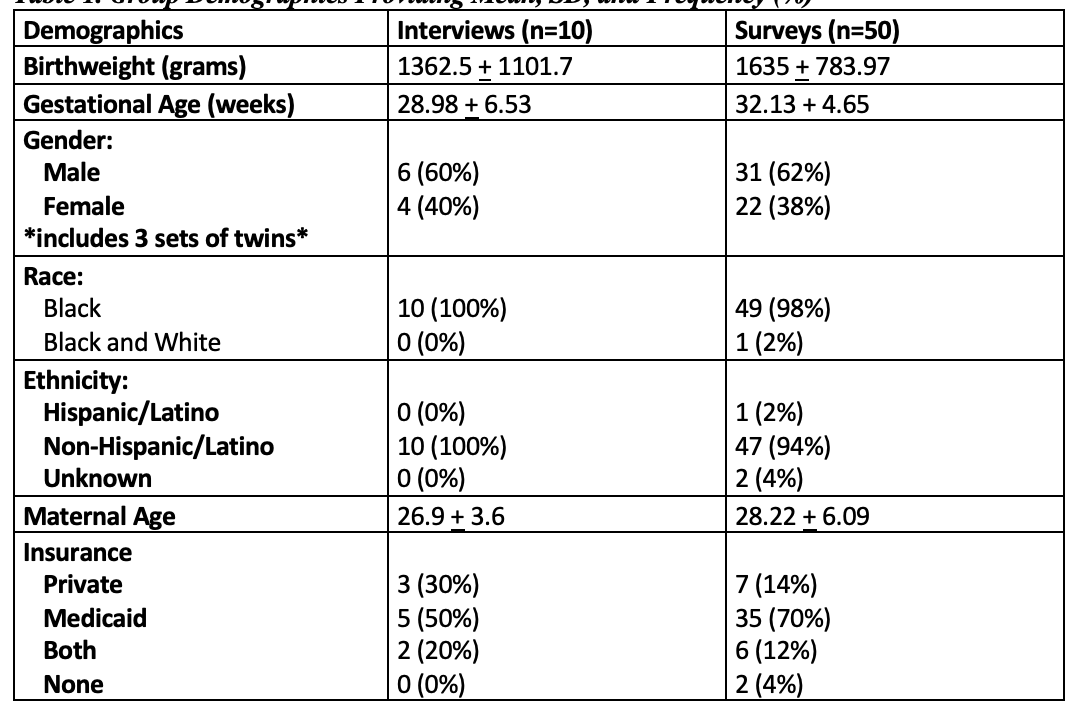
It is well known that Black mothers of healthy term infants face different obstacles to successful long-term lactation than White mothers. They have the lowest rates of breastfeeding initiation (60%) and continuation at 6 months (28%). Black infants in the Neonatal Intensive Care Unit (NICU), are less likely to receive Mothers Own Milk at discharge (23.1%). However, little is known regarding the lactation experiences of Black mothers of infant in the NICU who must use a breast pump to obtain milk for infants too premature or ill to breastfeed. It is important to have information on these unique challenges to develop interventions that would help in improving lactation success of Black mothers of infant in the NICU. The objective of this study was to explore the experiences of pump-dependent Black mothers of critically ill infants in the NICU including potential barriers and facilitators of successful lactation. In this mixed method study, mothers who identified as Black and had been pumping for > 7 days were interviewed (n=10) or surveyed (n=50) regarding their pumping experiences. Survey and interview guide questions were developed based on extensive literature review, feedback from lactation and disparity experts, and pilot tested with Black mothers in the NICU. Surveys were collected using Qualtrics and analyzed using simple statistic numbers and percentages. Interviews were conducted in a consult room, audio recorded, and then transcribed and analyzed using Atlas Ti, a qualitative research tool used for coding and analyzing transcripts. Greater than 60% of participants stated they struggled to meet their lactation goals. Barriers to successful lactation included access to breast pumps following discharge, time management due to other responsibilities, and insufficient communication with providers regarding lactation. In addition, mothers felt there was a lack of inclusive and culturally tailored lactation education by providers. Finally, mHealth technology, such as applications used to track pumping volume and frequency, was seen by participants as a tool to promote lactation success. To improve lactation success among Black mother of infants in the NICU, lactation education needs to be inclusive, accessible, and thorough. Strategies to facilitate access to hospital grade breast pumps is essential to promote lactation. Finally, mHealth technology is a promising intervention to help mothers reach their lactation goals.
Objective:
Design/Methods:
Results:
Conclusion(s):