Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 2: Epi/HSR Equity
631 - Racial disparities in genetic testing utilization in the NICU
Publication Number: 631.141

Marina Metzler, DO (she/her/hers)
Pediatric Resident
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background:
Neonates with genetic disorders are overrepresented in neonatal intensive care units (NICUs). With rapid genome sequencing, genetic testing is increasingly important in neonatal critical care. Racial disparities in access to genetic testing are well documented in ambulatory settings and, to a lesser extent, in NICUs with restrictive utilization review.
Objective:
To assess racial disparities in genetic testing utilization amongst neonates admitted to NICUs without utilization review, where genetics evaluation is at neonatologist’s discretion.
Design/Methods:
Retrospective analysis of 26,326 neonates born 2010-2021 at a Nationwide Children’s Neonatal Network delivery center and admitted to the NICU. Neonates with common aneuploidies, cystic fibrosis and sickle cell disease (N=184) and from racial or ethnic groups with fewer than 100 members in the cohort (N=230) were excluded. The primary, binary, outcome was any genetic testing order during the index hospitalization. We performed multiple logistic regression to determine the relative odds of the primary outcome by race, adjusted for sex, ethnicity, absolute birth weight Fenton Z-score (BW-Z), and gestational age (GA).
Results:
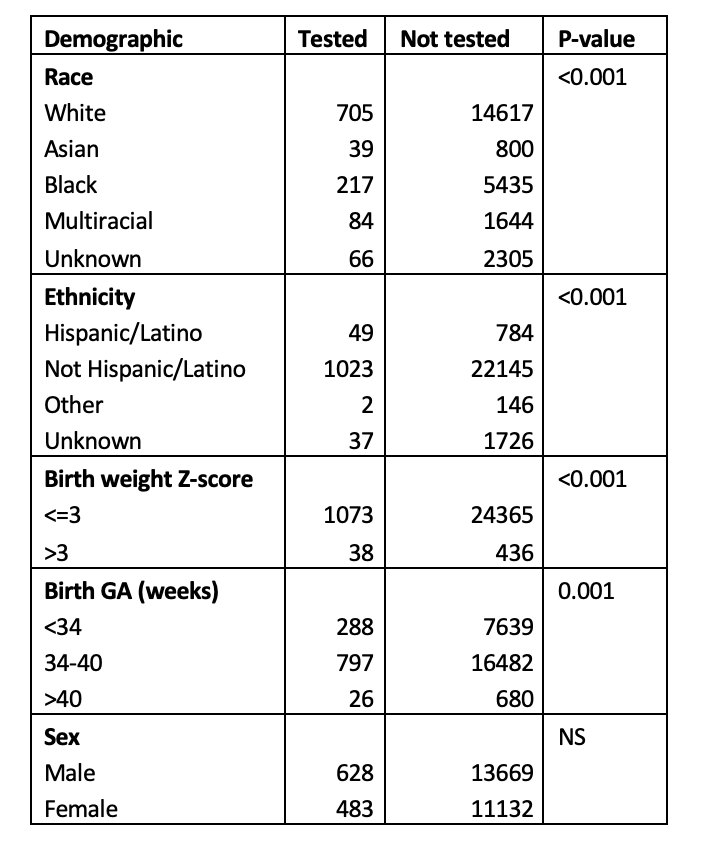
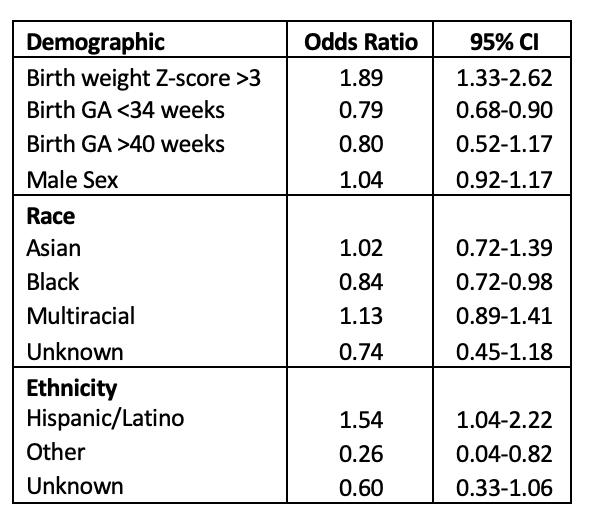
In univariate analysis, race, ethnicity, BW-Z and GA were all associated with the primary outcome (Table 1; Chi-square test). In multivariate analysis, Black neonates had lower odds of the primary outcome (OR=0.84, 95% CI 0.72-0.98) vs. White neonates. Hispanic/Latino neonates had higher odds (OR=1.54, 95% CI 1.04-2.22), neonates with high BW-Z had higher odds (OR=1.89, 95% CI 1.33-2.62) and those born prior to 34 weeks had lower odds (OR=0.79, 95% CI 0.68-0.90) of the primary outcome (Table 2).
Conclusion(s):
Black neonates were less likely to have genetic testing than White neonates. Premature neonates were tested less often while those with more extreme BW Z-score were tested more frequently. Strengths include large sample size, complete ascertainment of the outcome of interest and inclusion of a near complete geographic birth cohort. Limitations include lack of post-discharge testing data and inability to disentangle effects of biased referral patterns from our main effect, though a sensitivity analysis suggests minimal bias in referral to the Level IV center within our Neonatal Network. Without a biologically plausible reason to suspect a genetic diagnosis less often in Black neonates, the differences observed are likely due to implicit bias and/or structural racism. While parents may decline testing, differences in uptake of genetic testing by race, should they exist, may reflect medical mistrust.