Quality Improvement/Patient Safety: Evaluation Research on QI Educational Interventions
QI 1: Improvement Science Research Methods & Evaluation of QI Educational Interventions
674 - Improving the Use of Medication Health Literate Teaching Techniques to Ensure Safe Discharge from the ED
Publication Number: 674.151

Austin Gerdes, MPH (he/him/his)
Medical Student
Medical College of Wisconsin
Greenfield, Wisconsin, United States
Presenting Author(s)
Background:
Caregivers frequently mis-dose medication causing harm and utilization of healthcare. Evidence-based teaching techniques such as using teach-back, plain language, and open-ended questions can prevent harm from misunderstanding. Few Quality Improvement (QI) efforts have focused on evaluating and improving medication teaching techniques.
Objective:
To improve the percentage of health literate teaching techniques used during ED discharge.
Design/Methods:
An improvement team determined drivers of patients receiving quality discharge medication teaching. Workflow diagrams, value stream map, and cause and effect diagrams aided in planning. Interventions included workflow improvement, physician, APP, and nursing training on best practices, Meducation® was implemented in the EHR system which provided pictograms, and boost trainings at staff meetings.
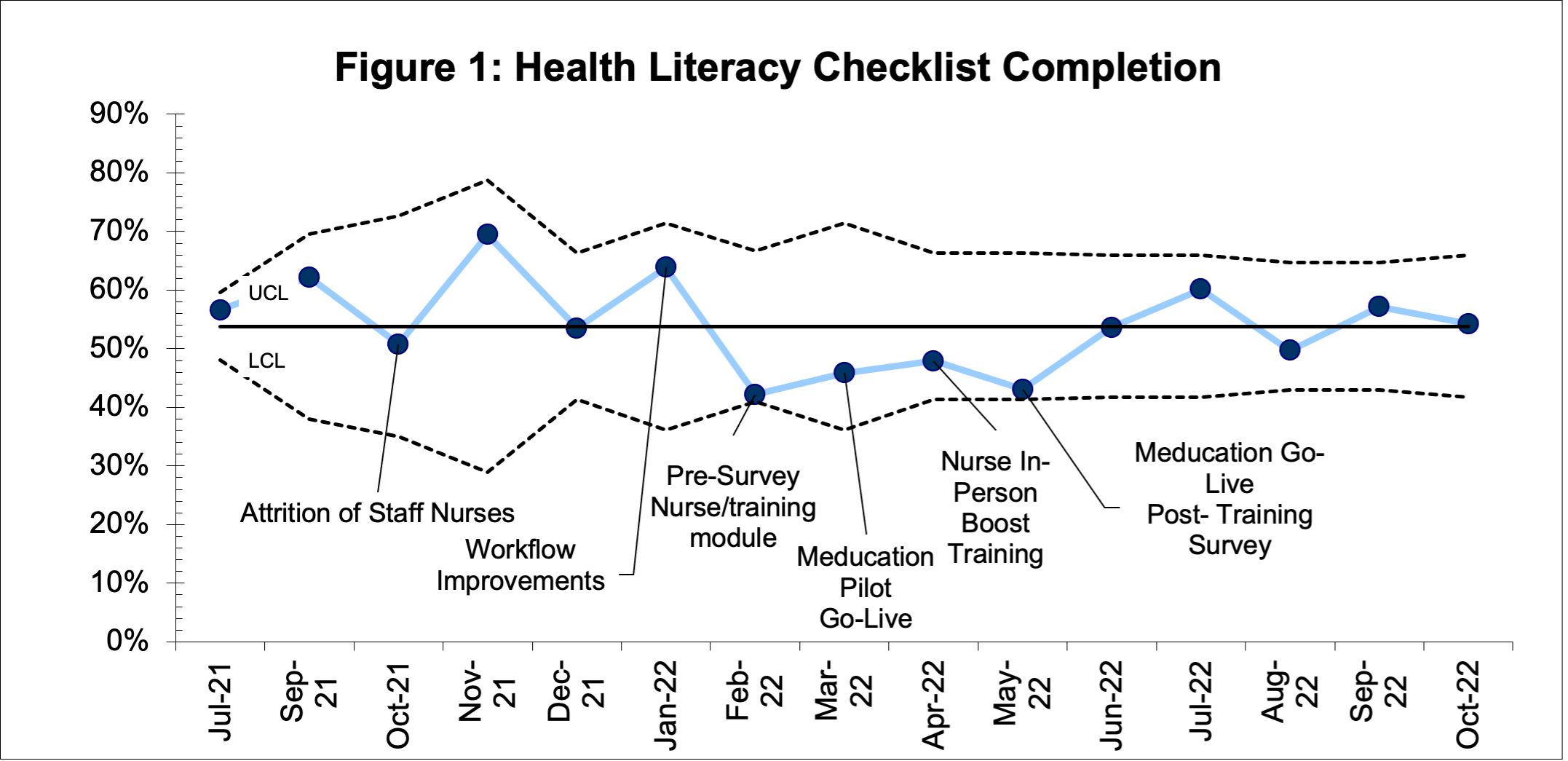
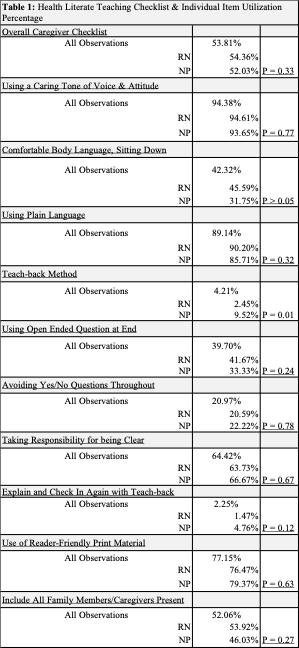
A trained observer completed a discharge observation checklist including discharging staff role and health literate teaching techniques from the Always Use Teach back checklist. Analysis included the percentage of each checklist component, and all components as overall percentage of the checklist completed. The percent of discharges with the technique completed were followed on run and statistical process control charts (p-charts). Chi-square tests were used to compare the proportions of Staff Nurse vs. NP completing discharge elements.
Results:
A total of 267 discharges were observed and evaluated using the developed medication teaching checklist. During the implementation period, a “Helping Hands” program consisting of mainly NPs began to aid with discharges in a high turnover areas of the ED during times of staff attrition and high ED volumes. A total of 204 discharges by RNs and 63 by NPs were observed.
Overall, 53.8% of the elements of the health literate teaching checklist were completed. There was no significant trend over time during the study period. The teach-back method was only observed 11 times (4% of discharges) and use of a pictogram 2 times (< 1% of discharges). When comparing RNs vs the NPs in the discharge specific role, NPs were found to use the teach-back method more often than the staff RNs (9.5% vs 2.5%, p< 0.05).
Conclusion(s):
There was not a significant trend in the utilization of health literate teaching techniques over time. An important technique for safety, teach-back, was infrequently used even after interventions. Notably, the dedicated discharge role used the teach-back method more often demonstrating the benefit of role clarity and having time and tools needed for ED teaching, which could include a discharge role.