Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 1: GI Health and NEC Complications
329 - Mucous Fistula Refeeding in Neonates: A Systematic Review and Meta-analysis
Publication Number: 329.133

Gonzalo Solis-Garcia, MD (he/him/his)
Fellow
THE HOSPITAL FOR SICK CHILDREN
TORONTO, Ontario, Canada
Presenting Author(s)
Background:
Mucous fistula refeeding (MFR) aims to maximize bowel function when an ostomy is active after abdominal surgery, by introducing the proximal ostomy effluent into the distal mucous fistula to maintain intestinal physiology. Although the technique has been known for decades, evidence in neonates is limited and no meta-analysis has been conducted to date.
Objective: To systematically review and meta-analyze the effectiveness and complications of MFR in neonates following abdominal surgery.
Design/Methods:
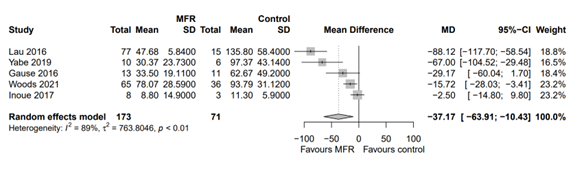
PubMed, Embase, Cochrane and CINAHL were searched till June 2022 for studies including neonates with ostomy receiving MFR compared to neonates with ostomy without MFR. The primary outcome was duration of parenteral nutrition. Pre-specified secondary outcomes were time to full enteral feeds, rates of cholestasis, and length of hospital stay. Subgroup analysis was performed for necrotizing enterocolitis (NEC) patients. Meta-analysis of pooled data was performed using random effects models given heterogeneity of studies, with Review Manager and R 4.1.0. The Risk of Bias in Non‐Randomized Studies of Interventions (ROBINS‐I) tool was used for risk of bias assessment and certainty of evidence was evaluated according to GRADE.
Results:
A total of 16 observational studies were included (N=623). ROBINS‐I tool showed moderate to serious risk of bias across the included studies. Compared to control group, neonates who received MFR had fewer days of parenteral nutrition [mean difference (MD) - 37.17 days, 95% CI -63.91 to -10.4, N = 244, 5 studies, GRADE: Low]. In addition, neonates who received MFR had lower rates of cholestasis (RR 0.46, 95%CI 0.36 to 0.59), shorter time to reach full feeds (MD -13.37, 95% CI -24.61 to -2.13) and shorter hospital stay (MD -55.12, 95% CI -102.21 to -8.03). In NEC patients, infants who received MFR had less cholestasis and shorter time to full feeds.
Conclusion(s):
Low certainty of evidence suggests that MFR is associated with shorter duration of parenteral nutrition in neonates following abdominal surgery and stoma creation. Adequately powered trials are needed to corroborate these findings.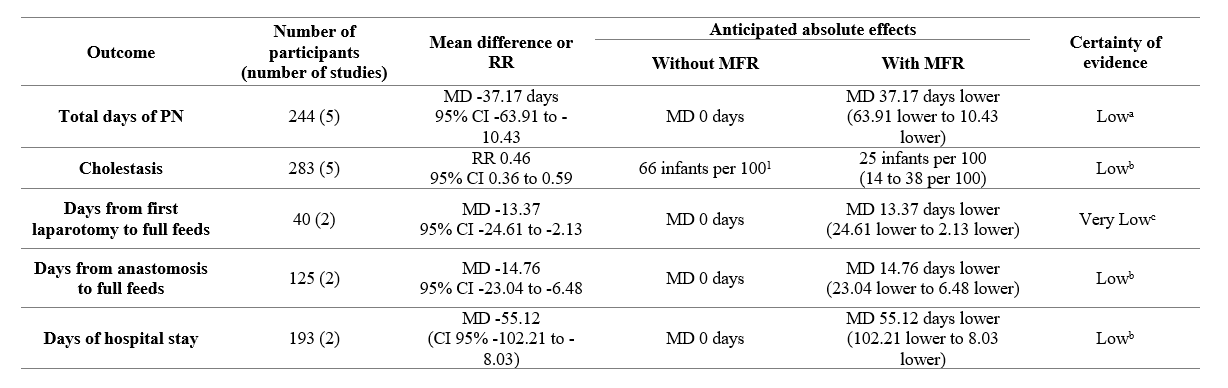
.png)
