Emergency Medicine: All Areas
Emergency Medicine 3
53 - Performance of blood biomarkers in febrile infants less than 3 months of age with very short duration of the fever
Publication Number: 53.112

Borja Gomez, MD, PhD (he/him/his)
Pediatric Emergency Physician
Cruces University Hospital
Barakaldo, Pais Vasco, Spain
Presenting Author(s)
Background:
Some recent studies show that half of the young febrile infants are seen at the pediatric emergency department (PED) in the first two hours of the duration of the fever. The performance of any clinical prediction rule for the management of febrile infants may be poorer in these infants. To our knowledge, the performance of biomarkers related to the duration of the fever to identify young febrile infants with an invasive bacterial infections (IBI) has not been analyzed.
Objective:
To analyze the performance of white blood cells count (WBC), absolute neutrophil count (ANC), C reactive protein (CRP) and procalcitonin (PCT) to identify febrile infants ≤90 days of age at risk for IBI, depending on the duration of fever.
Design/Methods:
We conducted a secondary analysis of a prospective single-center registry that includes all consecutive infants ≤90 days of age with fever without a source evaluated at the PED of a tertiary teaching hospital between 2008 and 2021. We excluded infants lacking data on duration of the fever, urine dipstick test results, urine culture obtained by a sterile method or blood culture; or blood CRP or PCT levels.
We defined IBI as the isolation of a bacterial pathogen in blood and/or cerebrospinal fluid. For the purpose of the study, we classified infants into 2 groups based on caregiver-reported hours of fever (< 2 and ≥2) and analyzed the performance of the biomarkers and of two commonly used clinical decision rules (PECARN and Step by Step).
Results:
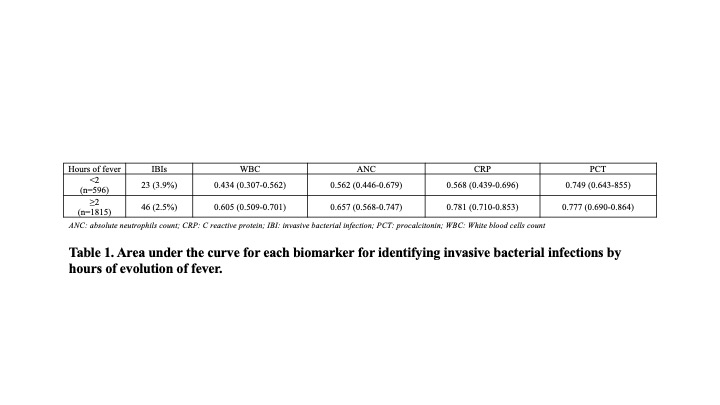
Of the 2993 registered infants, 2411 (80.6%) were included. Among them, 69 (2.9%) were diagnosed with an IBI (61 bacteremia, 4 meningitis and 4 meningitis with associated bacteremia). The median age was 52 (P25-P75: 33-68) days old, and the median duration of fever was 4 (P25-P75: 2-12) hours. In Table 1 we show the area under the curve for each biomarker for identifying IBIs by hours of evolution of fever.
The sensitivity of both Step-by-Step (82.7% vs 97.8%) and PECARN (87.0% vs 91.3%) rules decreased also in the first 2 hours.
Conclusion(s):
Management of febrile young infants with a very short duration of fever should be more cautious. The performance of blood biomarkers, except for procalcitonin, in febrile young infants decreases in these infants and this may alter the performance of different clinical prediction rules. Larger multicenter studies are needed to confirm these results.