Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 2: Gut and Liver Health
345 - Antibiotic exposure in first week after birth among premature neonates is associated with necrotizing enterocolitis and poor in-hospital growth
Publication Number: 345.134

Katie M. Strobel, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Washington School of Medicine
Maple Valley, Washington, United States
Presenting Author(s)
Background:
Antibiotic administration for less than three days in premature and term neonates directly alters the gut microbiome with effects potentially lasting for years. There is growing evidence that infants with necrotizing enterocolitis and growth failure have an altered microbial signature prior to these pathologies’ onsets. However, there are few studies examining the relationship between early postnatal antibiotic exposure with necrotizing enterocolitis and growth outcomes among premature neonates.
Objective:
To determine whether number of days of antibiotic exposure to extremely premature (EP, < 28 weeks) infants in the first week after birth is associated with necrotizing enterocolitis (NEC), cholestasis, and growth failure.
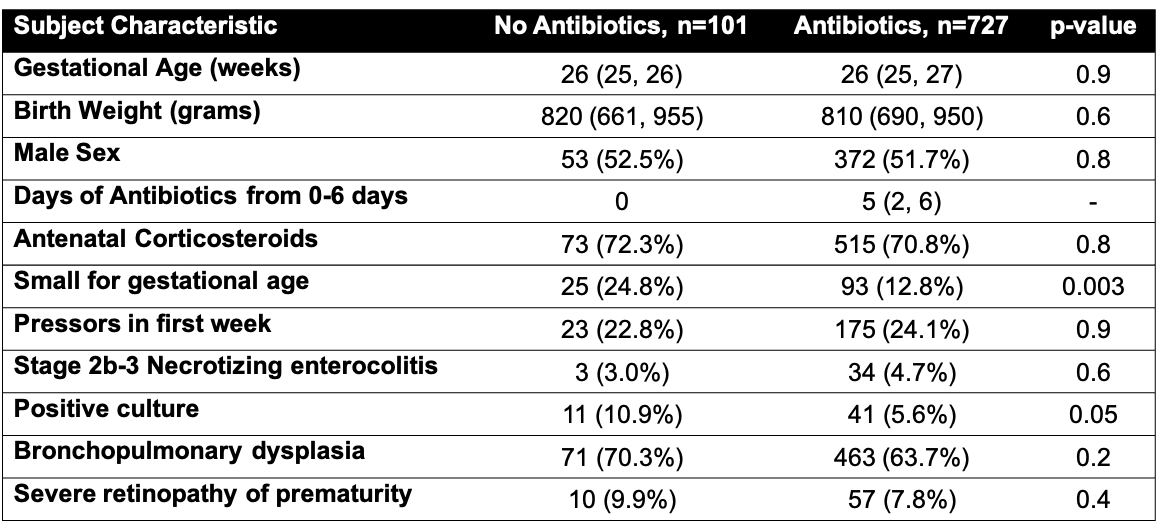
Design/Methods: This is a secondary analysis of surviving infants from the Preterm Erythropoietin (Epo) Neuroprotection Trial (PENUT Trial). Severe NEC was defined as Bell’s stage IIb or greater. All NEC episodes occurred after 7 days of age. Fenton growth curves were utilized for growth parameters. Growth failure was defined as a weight or length z-score change from birth to discharge of £-0.8. Cholestasis was defined as a direct bilirubin >1. Multivariable linear and logistic regression models were performed to control for potential confounders. The following variables were included in all models: gestational age (weeks), birth weight z-score, antenatal corticosteroids, positive culture (blood, CSF, or urine), and vasopressors in the first week.
Results:
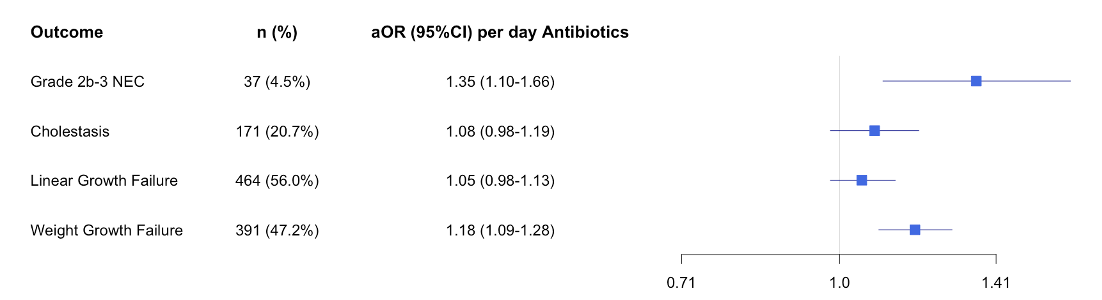
828 infants were included with a median (IQR) gestational age of 26 (25,27) weeks and birth weight of 810 (683,950) g. Cohort characteristics are shown in Table 1. When adjusting for confounders, increased antibiotic days in the first week was associated increased odds of developing severe NEC (aOR per day 1.35 [1.10, 1.66], p=0.0045) and weight growth failure (aOR per day 1.18 [1.09, 1.28], p< 0.0001) during the hospitalization. Increased antibiotics in the first week were not associated cholestasis (p=0.15) or linear growth failure (p=0.18) (Figure 1).
Conclusion(s):
Increased antibiotic exposure in the first week after birth was associated with increased odds of severe NEC and diminished weight growth during the hospitalization. Early antibiotic administration likely impacts the developing microbiome and intestinal tract. Further research should explore the early microbiota’s relation to necrotizing enterocolitis and poor growth.