Neonatal Fetal Nutrition & Metabolism
Neonatal Fetal Nutrition & Metabolism 1: Neonatal and Fetal Metabolism
298 - Risk of Neonatal Hypoglycemia in Infants of Mothers with Gestational Glucose Intolerance
Publication Number: 298.128

Chloe Andrews, MS, RD (she/her/hers)
Project Manager/PhD Student
Brigham & Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Gestational diabetes (GDM) increases risk of neonatal hypoglycemia (NH). The evidence regarding whether infants born to mothers with gestational glucose intolerance (GGI), or hyperglycemia that is below the threshold for GDM, are at increased risk of NH is sparse, mixed, and based on inconsistent research methods. In current clinical practice, infants are only screened for NH if they have a risk factor or symptoms, warranting further investigation into these associations to ensure that all at-risk infants receive appropriate screening and treatment.
Objective:
To examine the relationship between GGI and NH.
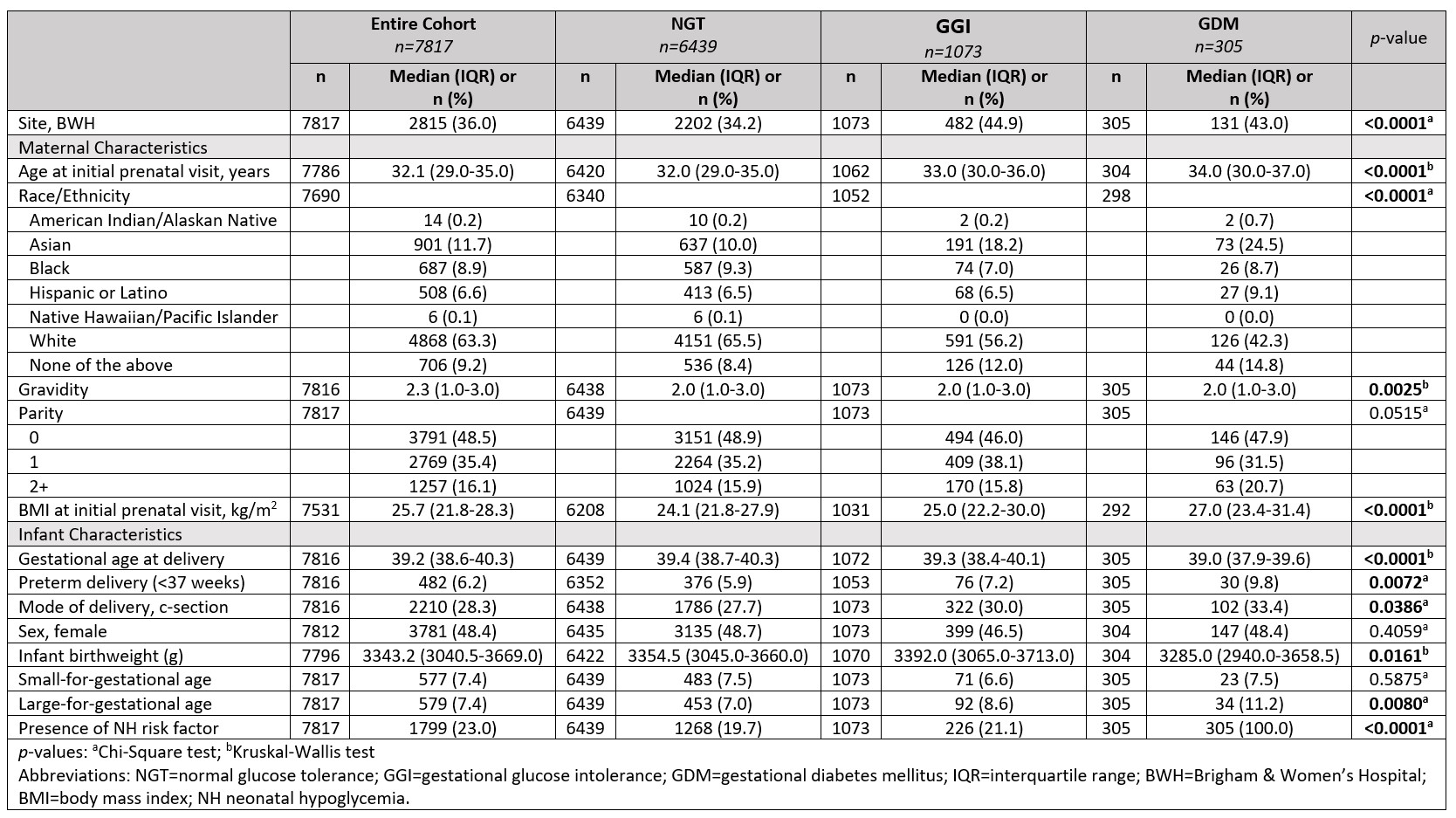
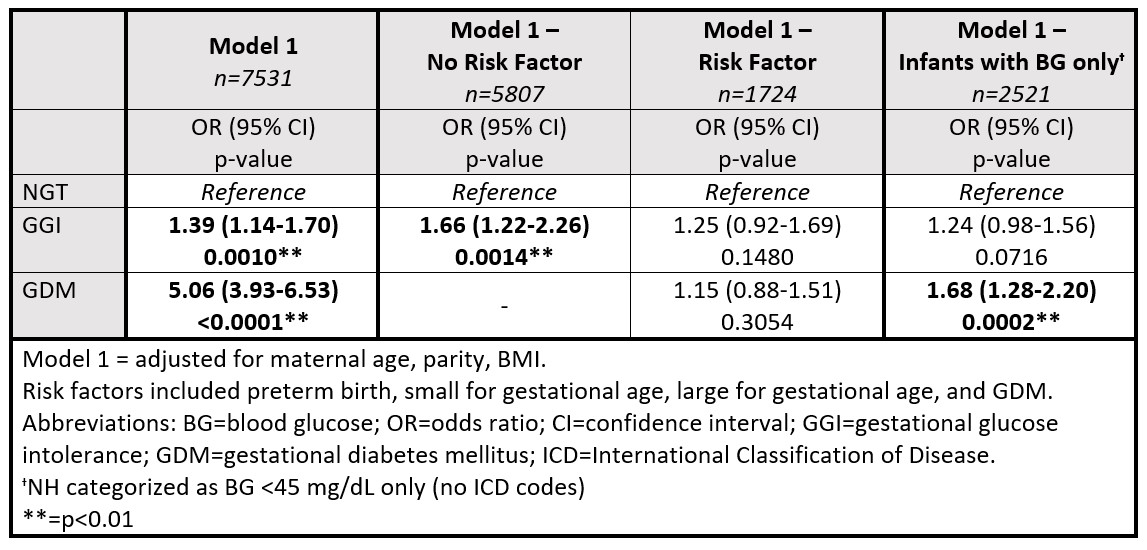
Design/Methods: This was a secondary analysis of electronic medical records-derived data of 7817 mother-infant dyads who delivered at two large, academic centers in Boston, MA between 2014-2022. The exposure was gestational glucose tolerance categorized as normal glucose tolerance (NGT), GGI-0, GGI-1, and GDM. We defined NGT as a normal glucose load test (GLT), GGI-0 and GGI -1 as a failed GLT with 0 or 1 abnormal values on the glucose tolerance test (GTT), and GDM as a failed GLT with ≥2 abnormal values on the GTT. Infants with a blood glucose (BG) < 45 mg/dL or an International Classification of Disease (ICD) diagnosis of NH were categorized as having NH. Infants without a BG measurement or an ICD diagnosis were categorized as normoglycemic. We used adjusted logistic regression analysis to determine associations between gestational glucose tolerance and NH. We performed stratified analyses by presence of a risk factor for NH (GDM, preterm, and/or small- or large-for-gestational age) and in infants with a BG measurement only.
Results:
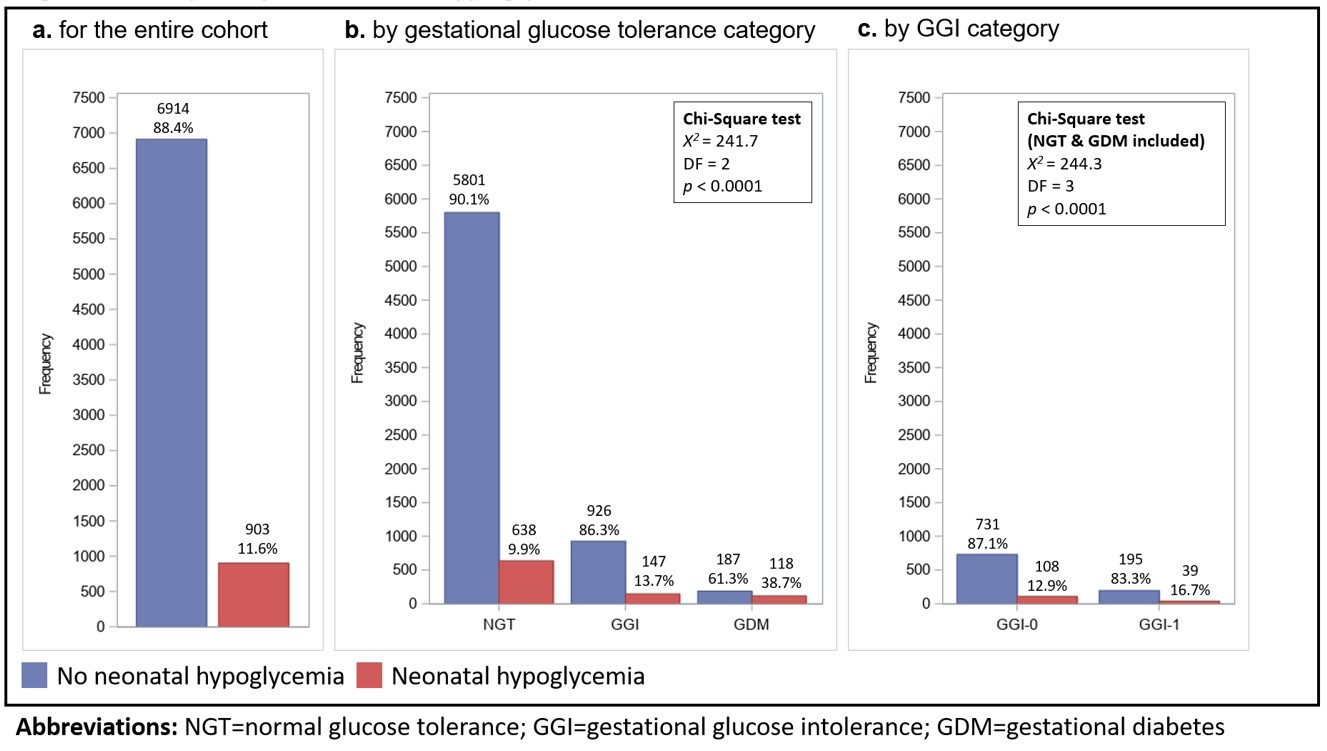
Maternal age, body mass index, rates of cesarean section, and preterm delivery increased across glucose tolerance categories (Table 1). Twelve percent of all infants had NH. The percentage of infants with NH increased across glucose tolerance categories (Figure 1). In fully adjusted models, infants born to mothers with GGI had 1.4-times (95% confidence interval (CI) 1.1-1.7) higher odds of NH compared to infants born to mothers with NGT. Associations were only significant in infants without a risk factor. Associations were attenuated to the null when infants without a BG measurement were excluded, although there was still a trend towards higher odds of NH (Table 2).
Conclusion(s):
GGI may be associated with increased risk of NH. Future research should examine these associations in a cohort with more complete neonatal glucose ascertainment and determine the clinical significance of these findings on long-term child health.