Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 1
511 - Prediction of Children’s High ED Use Based on Social Determinants of Health: Comparison of Model Performance with Fewer Predictors
Publication Number: 511.116

Richard Sheward, MPP (he/him/his)
Director of System Implementation Strategies
Boston University School of Medicine
Brookline, Massachusetts, United States
Presenting Author(s)
Background:
Recognition exists of children’s social determinants of health (SDH) & healthcare utilization linkages. Electronic health records (EHR) often lack SDH. Identifying key SDH underlying healthcare utilization can improve early identification of children at risk of high healthcare use while economizing data collection burden.
Objective:
Using predictive models for number of annual emergency department (ED) visits, we compared comprehensive vs. sparse specification performance of SDH predictors of high ED use.
Design/Methods:
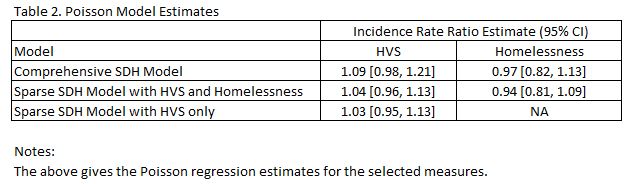
Longitudinal data (2007-2019) from families with children < 4 years interviewed in a Boston ED included a wide range of SDH predictors: food insecurity, Hunger Vital Sign (food insecurity risk; HVS) housing instability, homelessness, energy insecurity, difficulty with child care, & current public food assistance. EHR-linked survey data were used to obtain baseline (year 1 post-survey) & prospective (year 2 post-survey) ED visits & co-morbidities by ICD-10 codes. Outcome variable was number of ED visits in year 2. Using Poisson regression models we identified the top 5% of the children with the highest ED visits in year 2, varying the SDH predictor range added to complement the conventional EHR-based measures (age, sex, comorbidities, prior ED utilization). Using the model with all SDH included as the reference (comprehensive) we compared performance of sparse models including (a) HVS, & homelessness or (b) HVS alone. Sparse model performance was assessed in concordance with the top 5% of the sample identified from the comprehensive model. For model validation, the sample was randomly split into an estimation sample used to obtain prediction estimates & the validation sample for performance assessment.
Results:
Of 3,670 children, 33% were born to Hispanic mothers, 54% Black non-Hispanic, 7% White non-Hispanic, 6% other races/ethnicities. In year 2 post survey, ED visits ranged from 0 to 14, with a mean of 1.18. Prevalence of HVS was 43% & homelessness was 10%. Using the comprehensive SDH model, the top 5% of children (N=91) had 2.52 ED visits (mean). The sparse models with (a) HVS & homelessness, & (b) HVS alone identified 87% & 88% of the top 5% of children previously identified in the comprehensive model. HVS & homelessness coefficient estimates were not significant.
Conclusion(s):
Although a wide range of SDH are linked to healthcare utilization, SDH data collection can be burdensome. Our study indicates that prediction models to identify children at risk of high ED utilization may be adequate with a sparse set of SDH measures, in particular, HVS & homelessness..jpg)