Breastfeeding/Human Milk
Breastfeeding/Human Milk 2: Addressing Inequities in Lactation
374 - The Use of Telelactation to Decrease Disparities in Access to Outpatient Breastfeeding Support
Publication Number: 374.102

Melissa E. Glassman, MD, MPH, IBCLC (she/her/hers)
Associate Clinical Professor
Columbia University Vagelos College of Physicians and Surgeons
Columbia University Irving Medical Center
New York, New York, United States
Presenting Author(s)
Background:
Patients from low-income, minoritized communities have limited access to outpatient breastfeeding support with International Board Certified Lactation Consultants (IBCLCs). Telelactation may increase access particularly when appointments can be self-scheduled.
Objective: To describe a medical center-based, outpatient breastfeeding support program that includes telelactation and serves a diverse patient population.
Design/Methods: A retrospective electronic chart review was performed for patients with in-person or telelactation visits between April 2020-December 2021. Impact of demographics (language, race/ethnicity, insurance) on scheduling patterns (self-scheduled vs. traditionally scheduled), visit reasons, and impact of initial visit type and reason on the number subsequent follow up visits were determined using chi-square, paired t tests and linear regression as applicable.
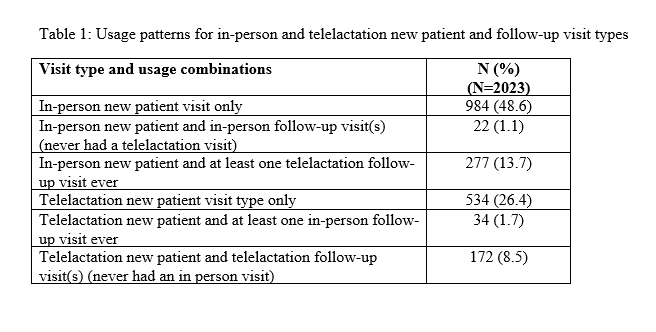
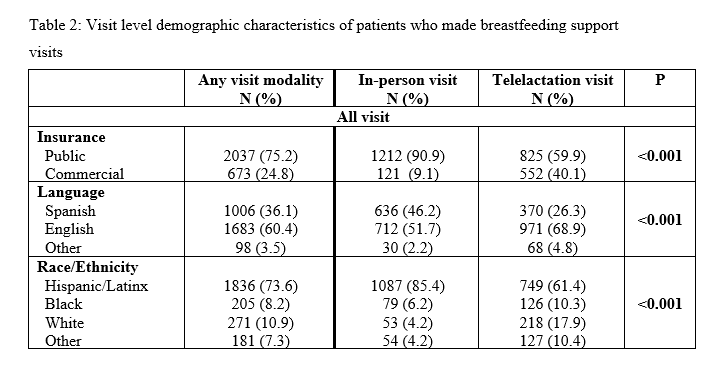
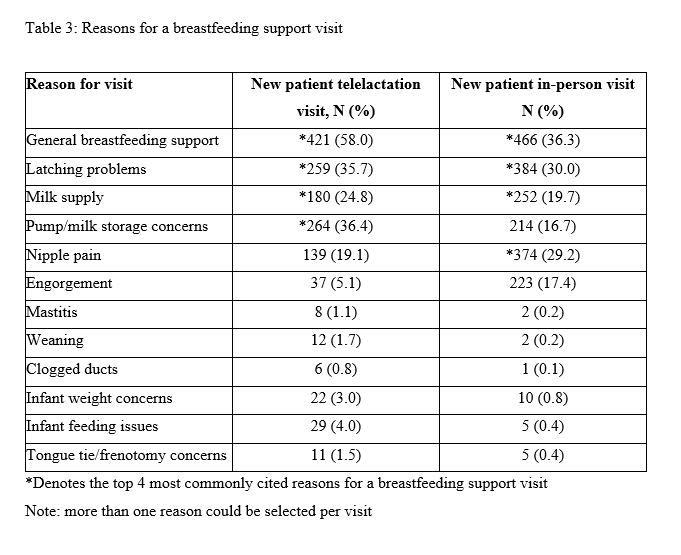
Results: Overall, 2023 patients made 2,791 visits (60.4% English-speakers, 73.6% self-identified as Latinx and 8.2% as Black, 75.2% publicly insured), of which 50.6% were for telelactation. Both visit types were utilized in a variety of combinations (Table 1). Latinx and publicly insured patients made most telelactation appointments (61.4% and 59.9% respectively). English-speakers (68.9%) used telelactation more than Spanish-speakers (26.3%) or other language speakers (4.8%) (Table 2). Self-scheduling resulted in decreased no show rates (25.3% vs. 42.8%, p< 0.001). Commercially insured patients had greater odds of self-scheduling vs. publicly insured (aoR 9.22 95% CI (6.27-13.57)) with no impact of race/ethnicity or language. Reasons for initial visit differed slightly by visit type (Table 3). On a stepwise linear regression model, reasons for initial visit that resulted in an increased number of follow-ups included infant weight concerns (Beta 0.59 95% CI (0.30-0.89), mastitis (Beta 0.80 95% CI (0.27-1.33), nipple pain (Beta 0.13 95% CI (0.043-0.22), and latching problems (Beta 0.09 95% CI (0.012-0.18). Telelactation as the initial visit type was also associated with a small increase in the number of follow-up visits (Beta 0.12 95% CI (0.038-0.19).
Conclusion(s):
Telelactation is a sought-after modality to address breastfeeding problems, including for publicly insured, Latinx and Black mothers who historically have had limited access to outpatient IBCLCs. Self-scheduling resulted in a lower no-show rate. Further support may be needed to best leverage telelactation among non-English speakers and self-scheduling for publicly insured patients.