Neonatal Neurology: Clinical Research
Neonatal Neurology 2: Clinical 2
162 - Does epidural analgesia increase the risk of hypoxic-ischemic encephalopathy (HIE) in the offspring?
Publication Number: 162.136

Marie-Coralie Cornet, MD, PhD (she/her/hers)
Assistant Professor, Division of Neonatology, Department of Pediatrics
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background:
Epidural analgesia is a cause of maternal hyperthermia, which is associated with an increased risk of neonatal brain injury. Yet, the relationship between epidural analgesia and neonatal hypoxic-ischemic encephalopathy (HIE) is unclear. Furthermore, it is unclear if elevated maternal temperatures due to epidural analgesia could lead to an increased risk of HIE.
Objective: To assess the association between epidural analgesia and neonatal hypoxic-ischemic encephalopathy.
Design/Methods:
In a large retrospective cohort of singleton term neonates born between 2012-2019 within Kaiser Permanente Northern California, we extracted from electronic medical records all maternal temperature measurements between 72 hours prior to delivery and 1 hour after delivery, duration of rupture of membranes, and presence and timing of epidural analgesia. We defined maternal hyperthermia as a single temperature >39C, or two or more temperatures >38C separated by at least 30 minutes. Our primary outcome of HIE was assessed by chart review of high-risk infants and defined as the presence of 1) neonatal encephalopathy that either a) persisted for >6 hours, b) was accompanied by seizures, or c) was treated with therapeutic hypothermia; and 2) acidosis defined as a cord gas ph< 7 or a base deficit in the first 2 hours after birth >10. We used logistic regression to evaluate the association between epidural analgesia and HIE, adjusting for confounders.
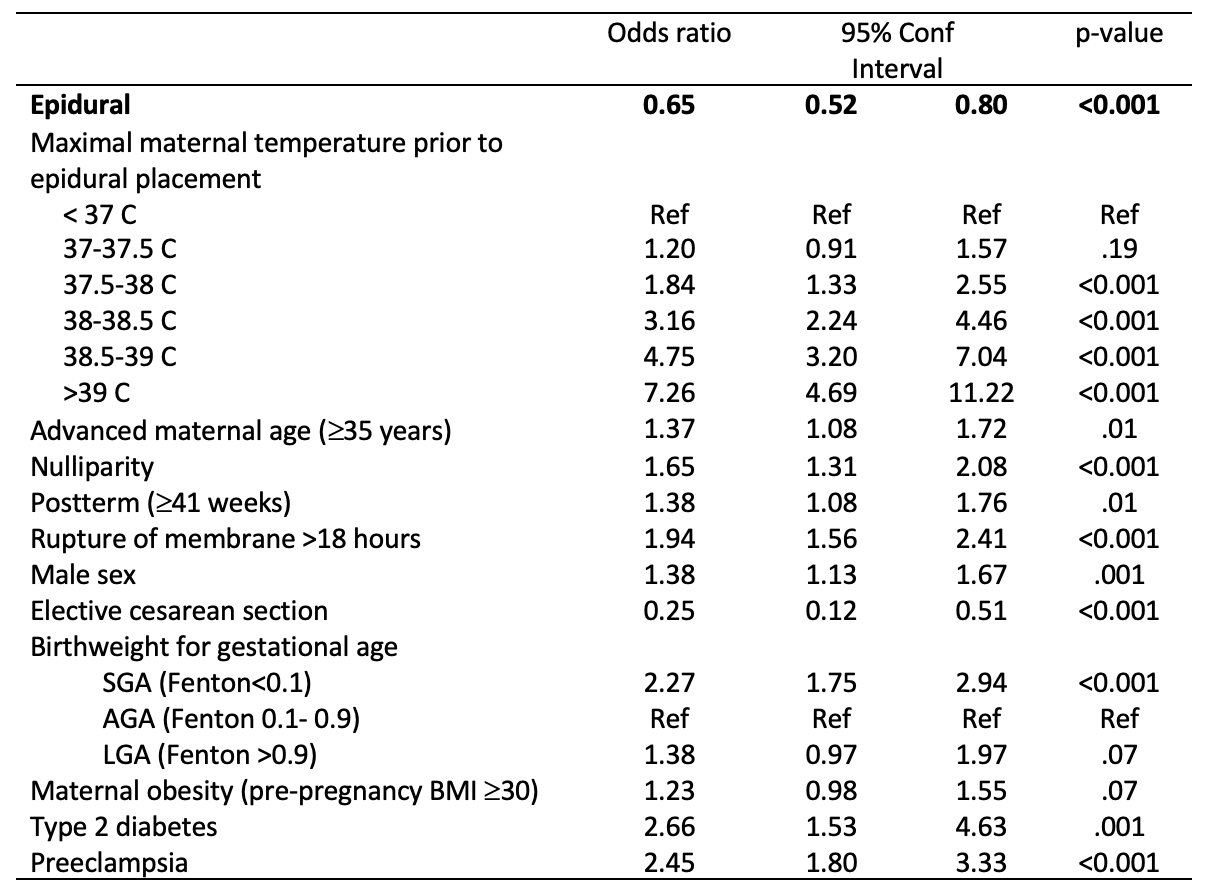
Results: Among 270,680 mother-infant dyads, 59% had epidural analgesia. 450 neonates had HIE (population incidence 1.7/1,000). In bivariate analysis, epidural analgesia was associated with an increased risk of HIE (RR 1.3, 95% CI 1.1-1.6). Epidural analgesia was also associated with an increased risk of maternal hyperthermia (RR 5.6, 95% CI 5.3-5.9), and neonates exposed to maternal hyperthermia had a higher risk of HIE (RR 5.5, 95% CI 4.3-6.8). However, when stratifying by the presence of fever, epidural analgesia was not associated with increased HIE rates (Table 1). Levels of several known risk factors for HIE varied among those who did and did not receive epidurals (Table 2). After adjusting for these potential confounders, including maternal temperature before epidural placement, epidural analgesia was associated with decreased odds of HIE (OR 0.6, 95% CI 0.5-0.8, Table 3).
Conclusion(s): While epidural analgesia increased the risk of maternal hyperthermia, the use of epidural analgesia was independently associated with a lower risk of HIE rather than an increased risk of HIE. Further studies are needed to confirm this finding, given the observational nature of our study.
.png)