Neonatal Follow-up
NICU Follow Up and Neurodevelopmental 2: Neonatal Growth, Nutrition and the Brain
207 - Neonatal hypernatremia and risk of long-term neurodevelopmental delay
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 207
Publication Number: 207.144
Publication Number: 207.144
Sandra Kumar, Texas A&M Health Science Center College of Medicine, Dallas, TX, United States; Taiwo Ojewole, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; irfan Shehzad, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Muppala Raju, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Madhava R Beeram, Texas A&M Health Science Center College of Medicine, Temple, TX, United States; Venkata Raju, Texas A&M Health Science Center College of Medicine, Temple, TX, United States; Vinayak Govande, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; MOHAMMAD N. UDDIN, Baylor Scott White McLane Children's Medical Center, Austin, TX, United States; Niraj Vora, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States
- SK
Sandra Kumar, B.A. (she/her/hers)
Medical Student
Texas A&M Health Science Center College of Medicine
Dallas, Texas, United States
Presenting Author(s)
Background: There is minimal information on the long-term effects of abnormal serum sodium levels in very low birth weight newborns, which may lead to higher morbidity and mortality. The purpose of this study was to look at the relationship between neurodevelopmental outcomes in children with very low birth weight and peak and baseline blood sodium levels.
Objective: To ascertain the strength, if any, of the relationship between neonatal hypernatremia and long-term neurodevelopmental outcomes.
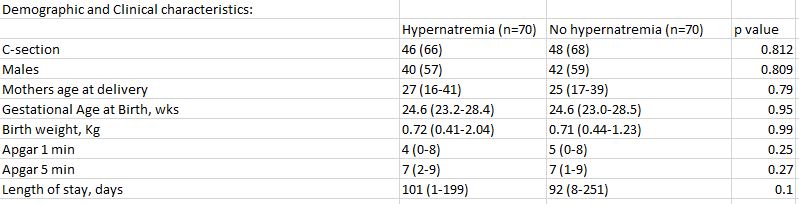
Design/Methods: Retrospective matched cohort study of infants born ≤ 28 wks at birth and admitted to the Baylor Scott & White Memorial hospital neonatal intensive care unit from January, 2010 to December, 2016 was conducted. Infants diagnosed with hypernatremia (plasma sodium level of ≥150mmol/L) and matched controls were included. Infants born at an outside hospital, readmitted after day of birth, with major congenital anomalies, endocrine disorders, or kidney injury were excluded. Additionally, infants that died before NICU discharge were excluded from the follow-up portion of the data collection/analysis. Primary outcome of developmental delay(s) measured using the objective Bayley scores of development. Demographic, clinical, and laboratory data were reviewed. Logistic regression was used to examine factors associated with neurodevelopmental delay.
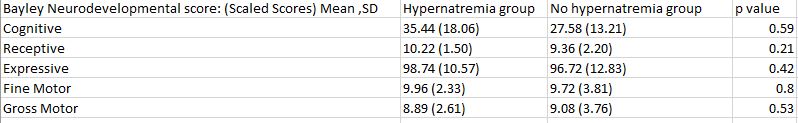
Results: 140 neonates were included: 70 with hypernatremia; 70 controls. Both median birthweight and median birth weight in both the groups were similar, 0.71 kg (range, 0.410-2.04) and 24.6 weeks (range, 23-28.5) respectively. There were no differences between cases and controls when comparing mode of delivery, sex, 1 and 5 minute Apgar scores, length of stay, or maternal age at delivery. In long-term follow-up, severe hypernatremia (plasma sodium level of ≥ 160 mmol/L) was associated with developing motor delay (p=0.0011), compared to infants with plasma sodium level 150-159mmol/L, and controls. There were no differences in the Bayley scores between the two groups.
Conclusion(s): There was no difference in the neurodevelopmental delay score as reported by the Bayley scale between the hypernatremia and the control group. Infants with severe hypernatremia are at increased risk for developing motor delay.