Neonatal General
Neonatal General 3: Ethics, Parents Take the Lead
283 - Change in Hospital Care of Newborn Infants with Trisomy 13
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 283
Publication Number: 283.132
Publication Number: 283.132
Allison O. Ignatz-Hoover, Cleveland Clinic Children's, Cleveland Heights, OH, United States; Anna Crist, Cleveland Clinic Children's Hospital, Cleveland, OH, United States; Mohamed A. Mohamed, Cleveland Clinic Children's, Cleveland, OH, United States; Hany Aly, Cleveland Clinic Children's, Cleveland, OH, United States
- AI
Allison O. Ignatz-Hoover, MD
Staff Neonatologist
Cleveland Clinic Children's
Cleveland Heights, Ohio, United States
Presenting Author(s)
Background: The outcomes of infants born with trisomy 13 have changed over recent years as more centers offer and perform procedures, particularly cardiac surgeries. Accordingly, the number of long-term survivors has increased.
Objective: To examine the change over recent years in neonatal survival to discharge, prevalence of adverse events, surgical procedures, tracheostomy and/or gastrostomy tube (g-tube) placement, and length of stay (LOS) in infants with trisomy 13.
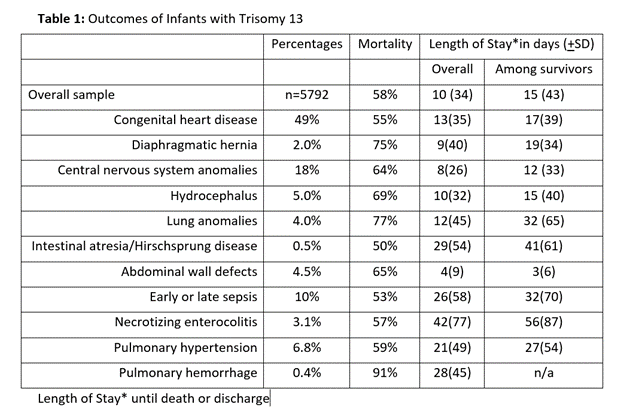
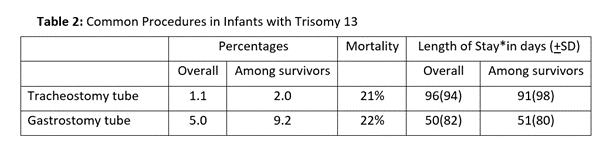
Design/Methods: We identified newborn infants diagnosed with trisomy 13 in the National Inpatient Sample (NIS), and its KID subversion, produced by the Health Cost and Utilization Project in the years 2003-2018. We calculated prevalence of commonly associated conditions such as congenital heart disease (CHD), diaphragmatic hernias, central nervous system (CNS), pulmonary or gastrointestinal (GI) anomalies, or abdominal wall defects (AWD). We examined procedures done, and common adverse events such as sepsis, necrotizing enterocolitis (NEC), pulmonary hemorrhage, or pulmonary hypertension, mortality associated with each condition, survival rates, and length of stay in overall sample and among survivors. We also calculated changes in trends over the years.
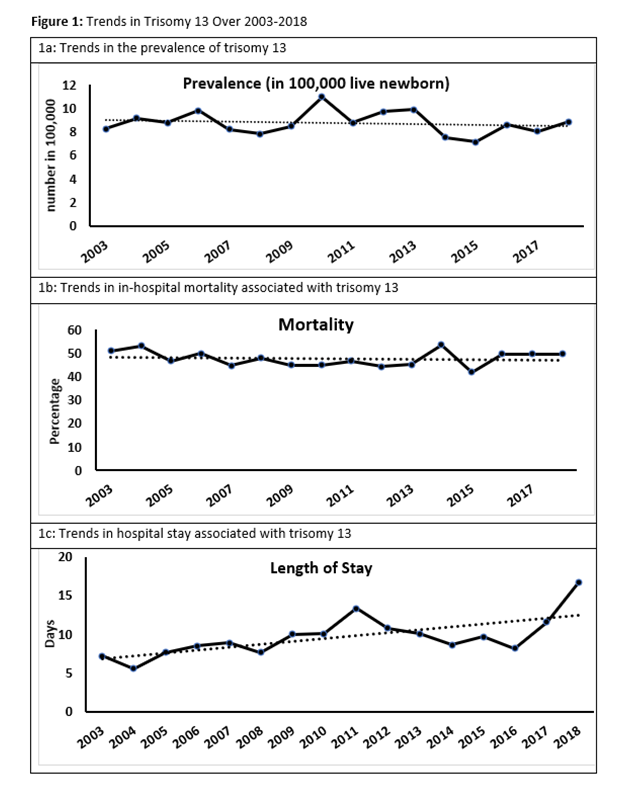
Results: Sample included 66,207,242 newborn infants. Of them, 5792 (0.01%) were diagnosed with trisomy 13 (8.7 in 100,000 live newborns). There was mildly significant decrease in the prevalence of trisomy 13 over the years (p< 0.001, Figure 1a). CHD were the most common associated anomaly (49%), followed by CNS anomalies (18%) and pulmonary hypertension (7%) (Table 1). Overall in-house mortality during neonatal period was 58%. There was no significant change in mortality trends over the years, (p< 0.001, Figure 1b). Mortality was highest among those with pulmonary hemorrhage, lung anomalies and diaphragmatic hernia (Table 1). Average length of stay was 10(+34) days. LOS had significantly increased over recent years (p< 0.001, Figure 1c). Average LOS was highest in conditions of NEC followed by gastrointestinal anomalies and sepsis (Table 1). Among survivors, 2% were discharged with tracheostomy and 9% with g-tubes. LOS was significantly increased in association with these procedures (Table 2).
Conclusion(s): There was a slight decrease in infants admitted to neonatal intensive care units with trisomy 13 over recent years. In-hospital neonatal mortality was unchanged. However, there was a significant increase in LOS, which was increased with procedures such as tracheostomy and g-tube placement, which may reflect a trend toward increasing interventions without a corresponding improvement in mortality.