Quality Improvement/Patient Safety: Evaluation Research on QI Educational Interventions
QI 1: Improvement Science Research Methods & Evaluation of QI Educational Interventions
671 - Implementation of Trauma Resuscitation Checklist to Facilitate and Evaluate Pediatric Readiness
Publication Number: 671.151

Elizabeth F. Horne, BS (she/her/hers)
Medical Student
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background:
Trauma is the leading cause of death and disability among children and adolescents. It is critical that trauma teams are prepared for the unique elements of pediatric trauma. Pediatric trauma activations are lower frequency compared to adult traumas, resulting in less exposure to pediatric trauma resuscitation during training. Pediatric readiness can be optimized through nuanced trauma training with standardized trauma scripts adapted for pediatric emergencies.
Objective:
To implement a standardized cognitive aid for pediatric trauma resuscitations and assess its impact on quality of care, teamwork, and cognitive load of trainees during monthly pediatric trauma resuscitation simulations and patient encounters.
Design/Methods:
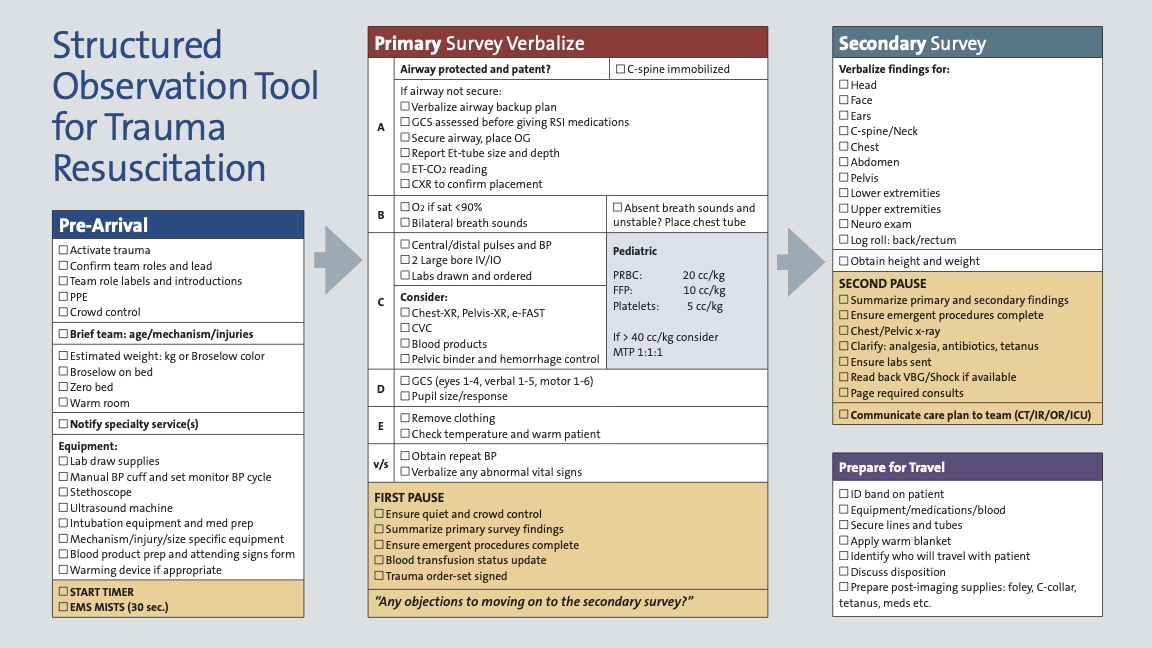
Using ACLS/ATLS guidelines and the ACS/ASE curriculum, we developed an institutional resuscitation bay trauma cognitive aid and structured observation tool (Figure 1) to act as stepwise trauma resuscitation script and a standardized evaluation tool. It is designed to facilitate prioritization of procedures and resuscitative elements, to create a shared understanding of the progression of the resuscitation among rapidly formed multidisciplinary teams, and to guide trauma education and debriefing. A monthly in-situ simulation program included multidisciplinary teams who completed an initial simulation, faculty then introduced the cognitive aid and used it to facilitate simulation debriefing and pediatric trauma specific education. The teams repeated the simulation to practice learning objectives and were re-assessed by the same group of evaluators. Participants completed a 15 question survey with components of the NASA Task Load Index and Team Emergency Assessment Measure after each simulation to assess the impact of the cognitive aid on cognitive load, teamwork, and quality of care. 7 pediatric trauma simulations with 100+ participants have been conducted since May 2021. Completeness of all indicated aspects of the checklist improved from a mean of 56.76% to 85.33%. Of 33 surveyed participants, 100% agreed that implementation of the cognitive aid reduced variability and improved teamwork and a reduction in reported cognitive load from 9 to 6 on a 21-point scale. Implementation of a standardized trauma checklist facilitates improved comprehensiveness of pediatric trauma assessments and reduced cognitive load during pediatric trauma resuscitation simulation. Multidisciplinary pediatric trauma simulations with a cognitive aid framework may improve teamwork, improve performance and reduce variability in both simulated and real pediatric trauma.
Results:
Conclusion(s):