Neonatal Follow-up
NICU Follow Up and Neurodevelopment 1: Developmental and Sensory Disorders
191 - Enhanced Prediction of Cerebral Palsy Using Brain Structural Connectivity Biomarkers at Term-Equivalent Age in Infants Born Preterm
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 191
Publication Number: 191.142
Publication Number: 191.142
Nehal A. Parikh, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Mekibib Altaye, Cincinnati Children's Hospital Medical Center, cincinnati, OH, United States; Karen Harpster, Cincinnati Childrens, Cincinnati, OH, United States; Julia Kline, National Institutes of Health, Bethesda, MD, United States; Armin Allahverdy, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Stephanie L. Merhar, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Weihong Yuan, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Nehal A. Parikh, DO, MS (he/him/his)
Professor of Pediatrics
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Despite recent advances in early diagnosis of cerebral palsy (CP), early detection based on imaging alone remains elusive and accurate methods for early prediction are urgently needed.
Objective: To improve CP prediction by exploiting diffusion MRI-based structural connectivity (SC) biomarkers in preterm infants.
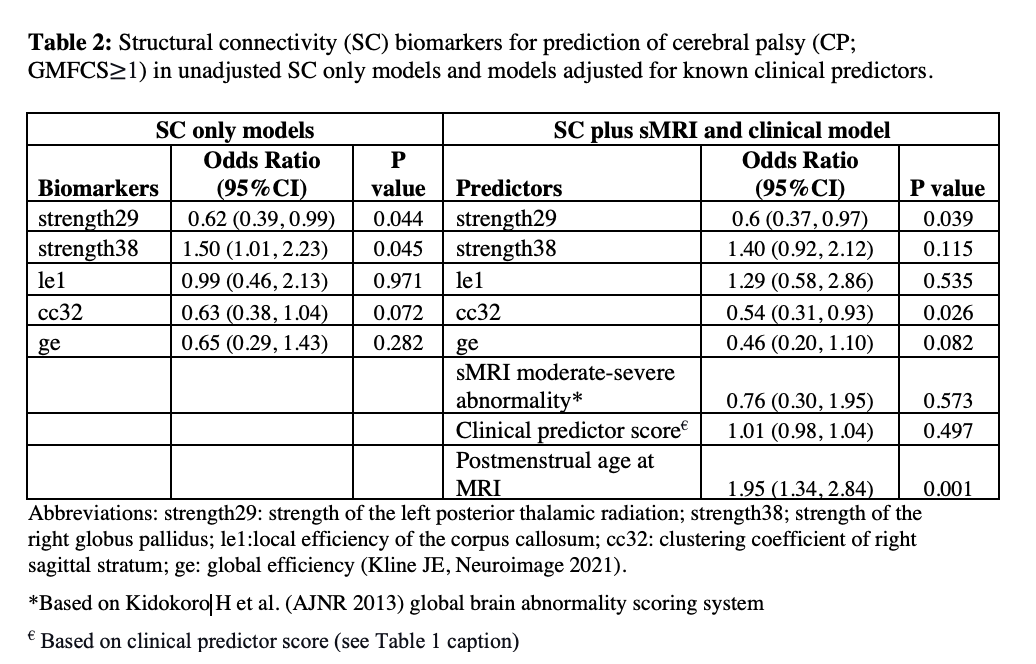
Design/Methods: We assembled a multicenter regional cohort of 345 preterm infants (≤32 weeks’ gestation) from 5 Southwest Ohio NICUs (CINEPS cohort). All infants were imaged at term-equivalent age (TEA) using structural and diffusion MRI on the same 3T Philips scanner and tested for CP at 2 years corrected age (CA) using the Amiel-Tison standardized neurological exam and the Gross Motor Function Classification System (GMFCS). Structural connectivity (SC) graph theory biomarkers were derived as previously reported (Kline JE, Neuroimage 2021). We created 500 bootstrapped datasets using random sampling with replacement from the original data. We cross-validated an elastic net model that selected the optimal penalty and L1/L2 ratio. We included 5 biomarkers that appeared in 90% of our bootstrapped models in a multivariable logistic regression model to predict CP at 2 years CA, over and above sMRI brain abnormalities and other known clinical predictors of CP (Table 2).
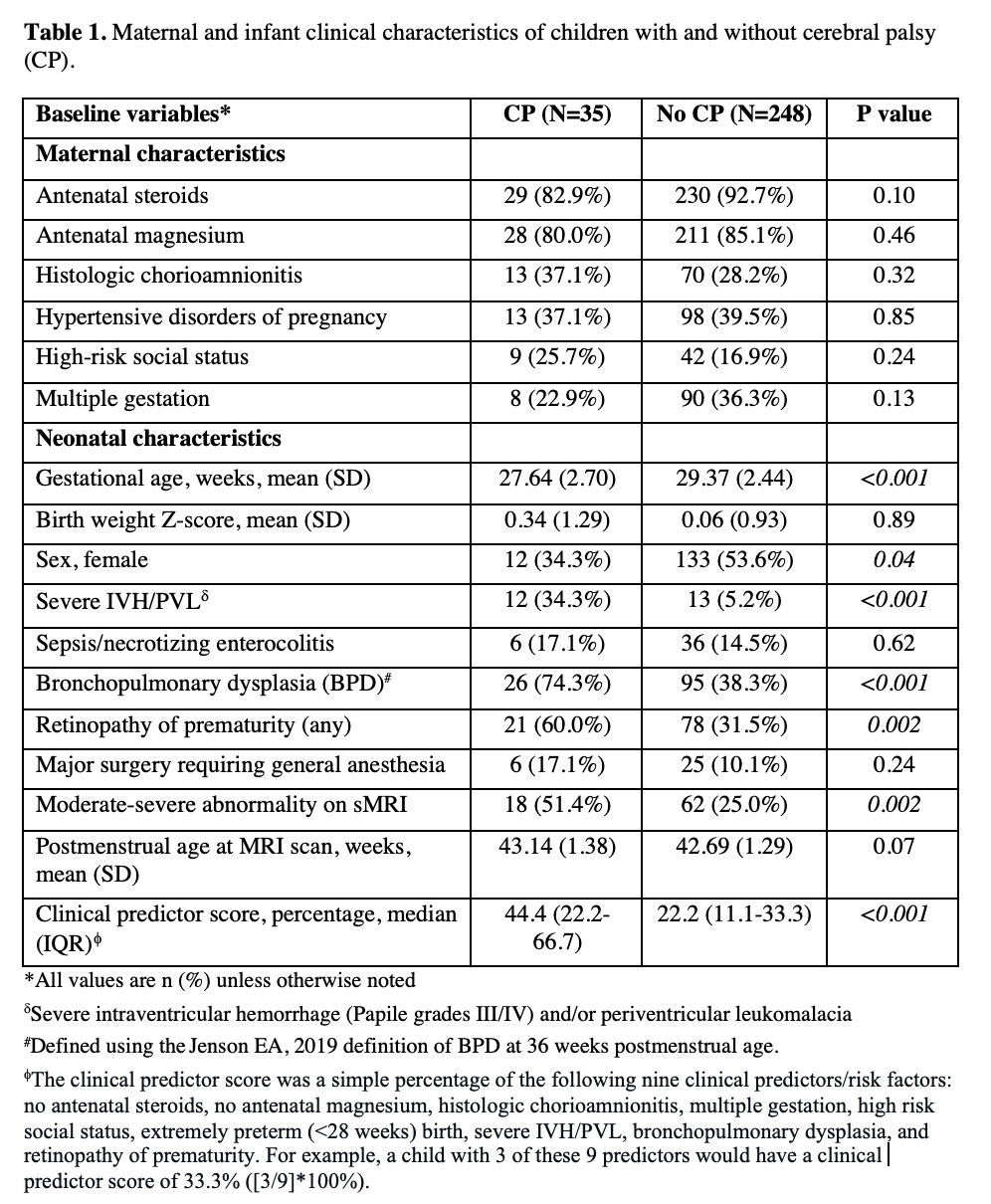
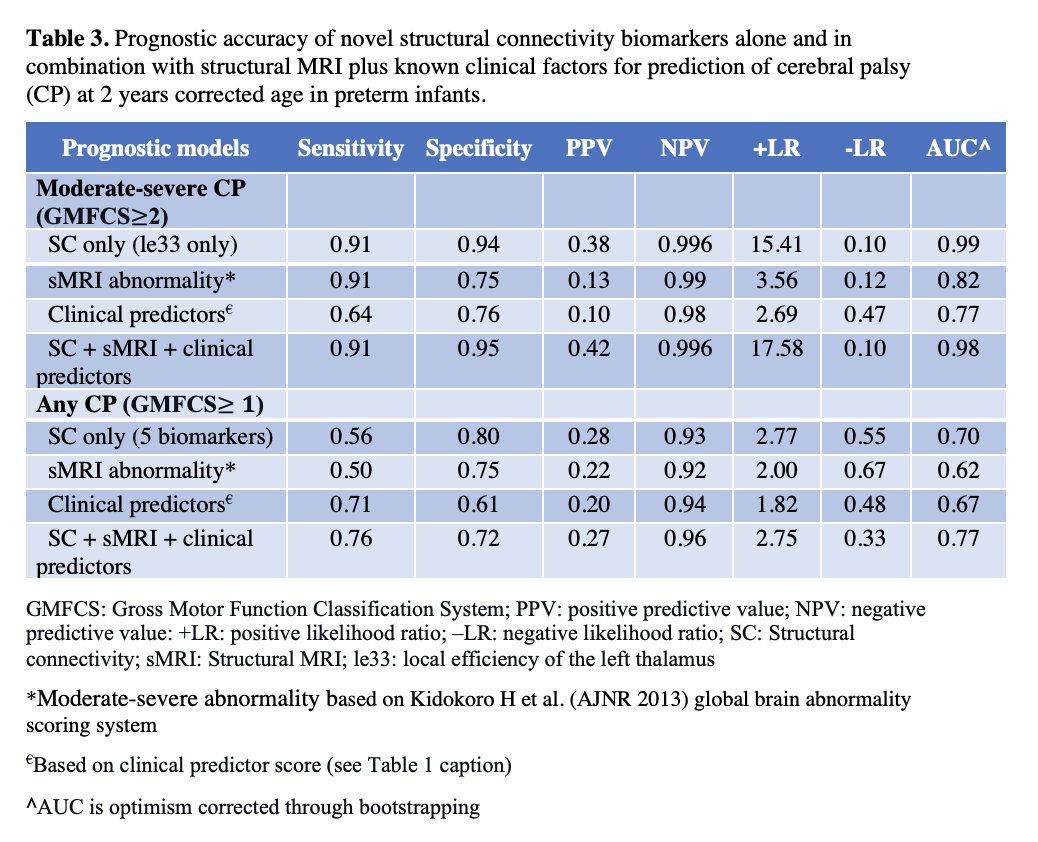
Results: Of the 345 infants, 332 had high quality dMRI data for analysis but 5 failed registration due to severe injury on sMRI (imputed lowest values for these cases). Of these, 283 infants (85%) returned for the 2-year follow-up and completed neurological testing; 35 (12.4%) were diagnosed with CP (GMFCS≥1), including 11 (3.9%) with moderate-severe CP (GMFCS≥2). The CP vs. non-CP groups differed in many clinical factors (Table 1). Two of the five SC biomarkers remained independent predictors of any CP in the combined multivariable models with other clinical predictors (Table 2). Only one biomarker, the local efficiency of the left thalamus, was sufficient to accurately predict moderate-severe CP (Table 3). The addition of SC biomarkers to existing clinical models considerably enhanced CP prediction accuracy (Table 3).
Conclusion(s): In a regional prospective cohort of high-risk preterm infants, we identified and internally validated the local efficiency of the left thalamus at TEA as a highly accurate biomarker for predicting moderate-severe CP. While prediction accuracy of any CP (inclusive of mild CP) was considerably higher than current clinical models, additional biomarkers are needed to improve prediction of mild CP.