Neonatal General
Neonatal General 3: Ethics, Parents Take the Lead
282 - Mode of Death in a Level IV NICU
Publication Number: 282.132
- CG
Catherine M. Groden, MD, MA (she/her/hers)
Neonatal-Perinatal Fellow
Indiana University School of Medicine
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background:
Approximately 20,000 US infants die every year, including 35-50 in our level IV neonatal intensive care unit (NICU). Nationwide, deaths in the NICU are more often occurring as a result of withdrawal (WD) or withholding of life-sustaining treatment, rather than in full codes. Factors associated with mode of death in the NICU are incompletely understood.
Objective:
Describe factors associated with mode of death in a level IV NICU.
Design/Methods:
Retrospective review of all infants who died in our level IV NICU or were discharged from the NICU on hospice care from 2017-2021. Infants who died in other hospital units or after non-hospice discharge from the NICU were excluded. Infants’ clinical characteristics, family characteristics, and end-of-life care data were collected. Infants who died after WD were compared to those who died after a code. Categorical factors were compared using chi-square or Fisher exact tests; continuous factors were compared using Mann-Whitney U test. P-values were adjusted for multiple comparisons.
Results:
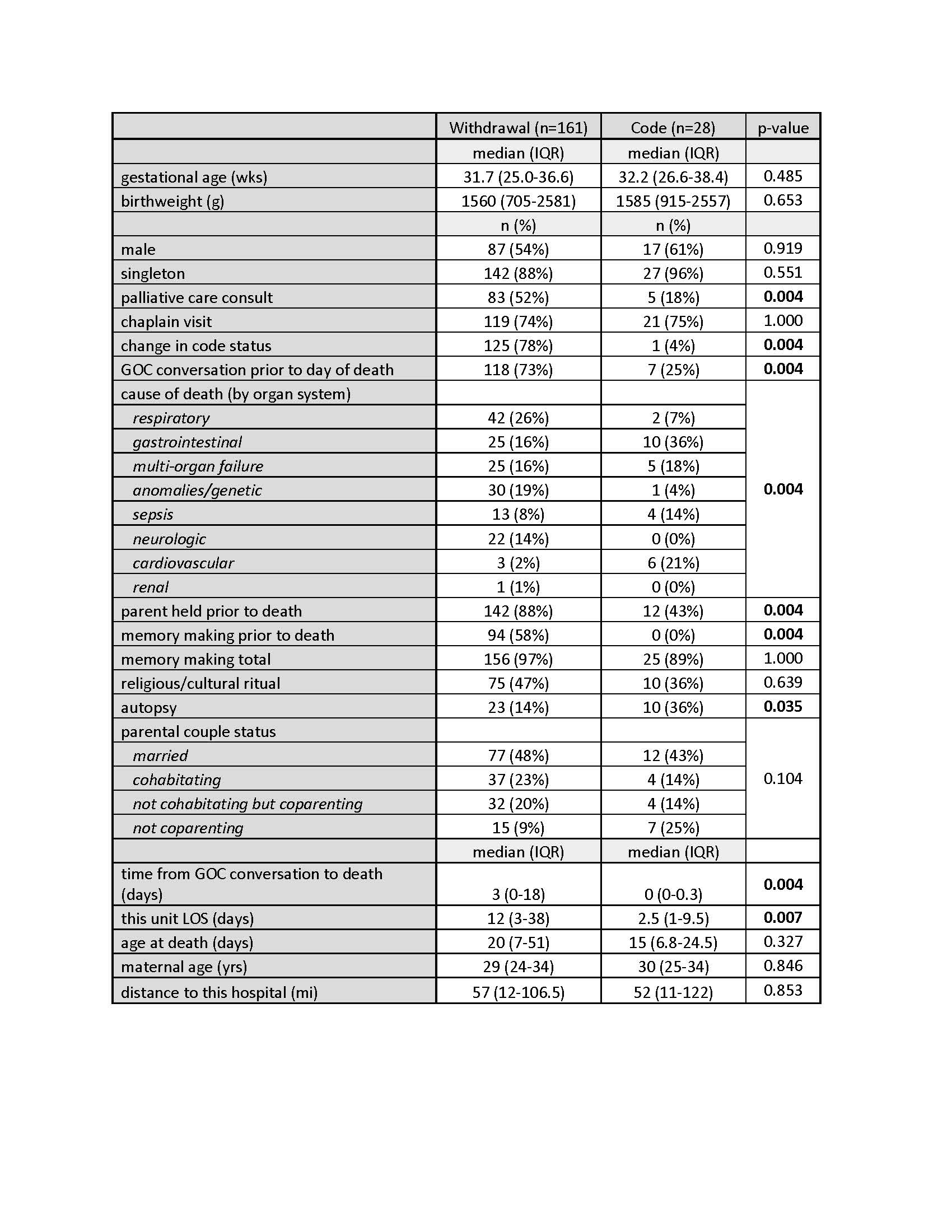
Out of 213 total infants, 161 (76%) died after WD; 28 (13%) died after a code. 24 infants (11%) died following some intermediate limitation of care. Details of the WD and code groups are in table 1. Gestational age, birthweight, and sex did not differ between the two groups. Compared to coded infants, infants who died after WD were more likely to have had palliative care consultations, to have had documentation of goals of care (GOC) conversations prior to the day of death, and to have been held by a parent prior to death. Infants who died after WD had longer length of stay in the level IV NICU and longer time between GOC conversations and death. Infants who died after a code were more likely to undergo autopsy. Cause of death varied between the two groups, with respiratory and neurologic causes more common in the WD group and GI and cardiovascular causes more common in the code group.
Conclusion(s):
Most infants who died in our level IV NICU did so after withdrawal of life-sustaining treatment. Palliative care consult, earlier goals of care conversations, and longer length of stay were associated with withdrawal. Autopsy was associated with death in a code.
This study adds to the limited existing literature on modes of death in the NICU. Some of our findings may be influenced by different severities of illness between the two groups; nevertheless, as end-of-life care practices continue to evolve, it is important to further our understanding of this deeply emotional topic.