Neonatal Fetal Nutrition & Metabolism
Neonatal Fetal Nutrition & Metabolism 1: Neonatal and Fetal Metabolism
297 - Prediction of Neonatal Hypoglycemia Risk from Maternal Continuous Glucose Monitoring Data Using Artificial Intelligence
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 297
Publication Number: 297.128
Publication Number: 297.128
Vivek Shukla, University of Alabama at Birmingham, Birmingham, AL, United States; Ashley N. Battarbee, University of Alabama at Birmingham, Birmingham, AL, United States; Ryan L. Melvin, University of Alabama School of Medicine, Birmingham, AL, United States; Ryan C. Godwin, University of Alabama at Birmingham, Winston Salem, NC, United States; Alan Tita, University of Alabama at Birmingham, Birmingham, AL, United States; Waldemar A. Carlo, University of Alabama School of Medicine, Birmingham, AL, United States; Akila Subramaniam, University of Alabama at Birmingham, Birmingham, AL, United States

Vivek Shukla, MD (he/him/his)
Assistant Professor
University of Alabama at Birmingham
Birmingham, Alabama, United States
Presenting Author(s)
Background: Neonatal hypoglycemia is a major complication in infants born to mothers with diabetes; delayed recognition can result in neurodevelopmental morbidities.
Objective: We sought to use an artificial intelligence (AI) framework to develop a prediction model to identify neonates at risk of hypoglycemia using maternal continuous glucose monitoring (CGM) data. The study hypothesis was that the model for identifying neonates at risk of hypoglycemia using maternal CGM data would have good predictive accuracy (area under the receiver operating characteristic curve, AUC >0.70).
Design/Methods: Retrospective cohort study of mother-infant pairs monitored using real-time CGM (Dexcom) during prenatal care who delivered at our center from 9/1/2018 to 3/31/2022. The primary outcome was neonatal hypoglycemia, defined by serum or point-of-care glucose measurements of < 40 mg/dl in the first 24 hours after birth. AI-based Multiple Representations Sequence Miner (MrSQM) framework was used to build the prediction model. Outcome stratified data were randomly split into 80% train and 20% test datasets. The predictive accuracy of the model was assessed on the test dataset using the AUC and area under the precision-recall curve (AUCPR).
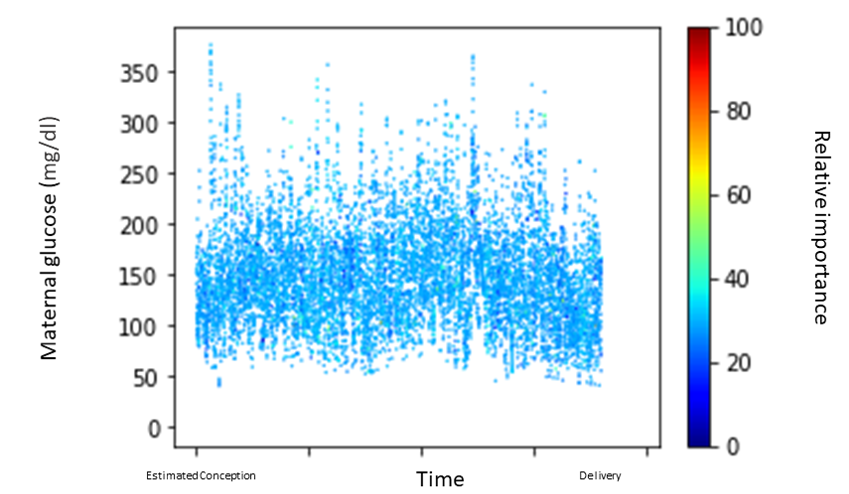
Results: A total of 90 mother-infant pairs were eligible and included in the study, of which 40 neonates (44%) had hypoglycemia. Baseline characteristics did not differ between neonates with hypoglycemia and those without (Table 1). The MrSQM saliency map (Figure 1), demonstrated low variance, indicating no single CGM reading was highly predictive; however, higher values were more important than lower values in the model’s prediction. The model prediction metrics were as follows: AUC of 0.74 and AUCPR of 0.81. Given the 56%/44% negative/positive class balance, the AUCPR of 0.81 indicates that the model has good predictive accuracy.
Conclusion(s): We developed an AI-based model with good predictive accuracy for neonatal hypoglycemia using maternal CGM data. Adding clinical variables may enhance predictive ability. Further studies should prospectively assess its implementation as a clinical decision support tool.
.png)