Neonatal Neurology: Clinical Research
Neonatal Neurology 2: Clinical 2
174 - Acoustic biomarkers of cries from newborns admitted to the NICU with hypoxic ischemic encephalopathy
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 174
Publication Number: 174.136
Publication Number: 174.136
Samantha Latremouille, Ubenwa Health, Montreal, PQ, Canada; Charles Onu, Ubenwa Health, Montreal, PQ, Canada; Junhao Wang, Ubenwa Health, Montréal, PQ, Canada; Arsenii Gorin, Ubenwa Health, Montreal, PQ, Canada; Wijdan Basfar, Mcgill university, Montreal, PQ, Canada; Adnan M. Al Ali, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Guilherme Sant'Anna, McGill University Health Center, MONTREAL, PQ, Canada
.jpg)
Samantha Latremouille, PhD
Co-founder & Clinical Development Lead
Ubenwa Health
Montreal, Quebec, Canada
Presenting Author(s)
Background: Newborns’ cries are involuntary reflexes controlled by the central nervous system. Thus, neurological injuries secondary to hypoxic ischemic encephalopathy (HIE) may alter acoustic biomarkers of cry.
Objective: To compare acoustic biomarkers of cries from newborns admitted to the NICU with HIE.
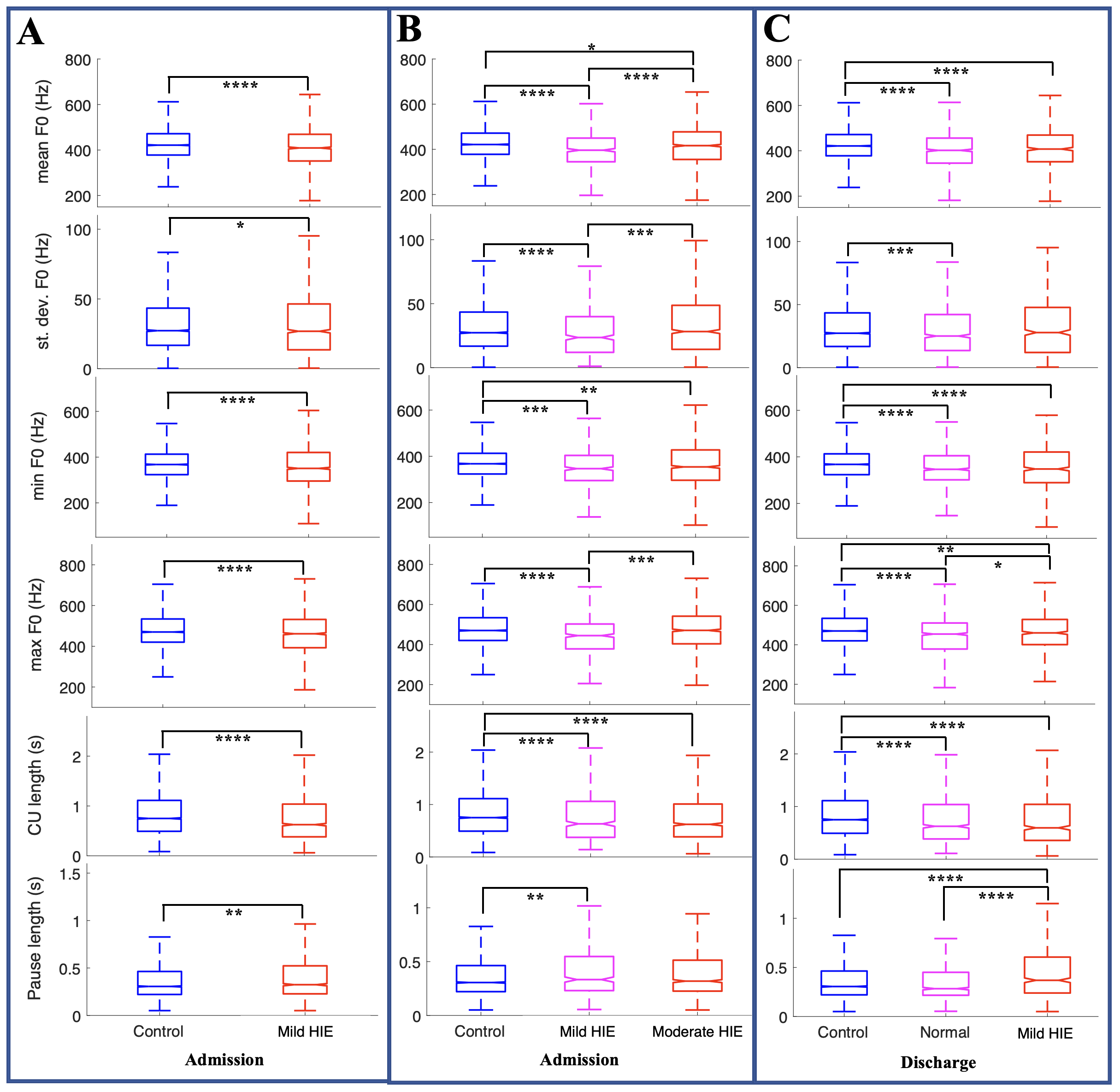
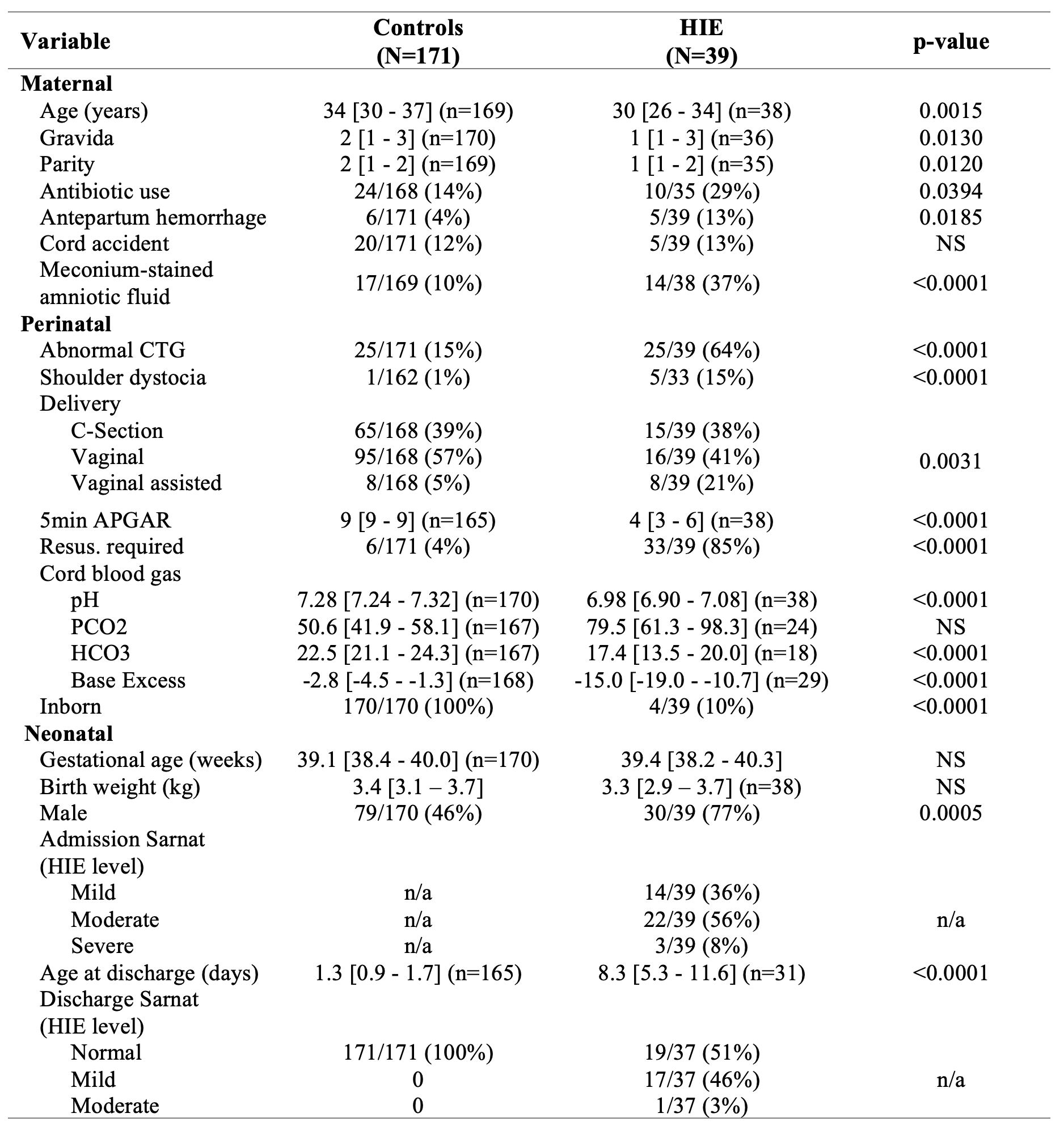
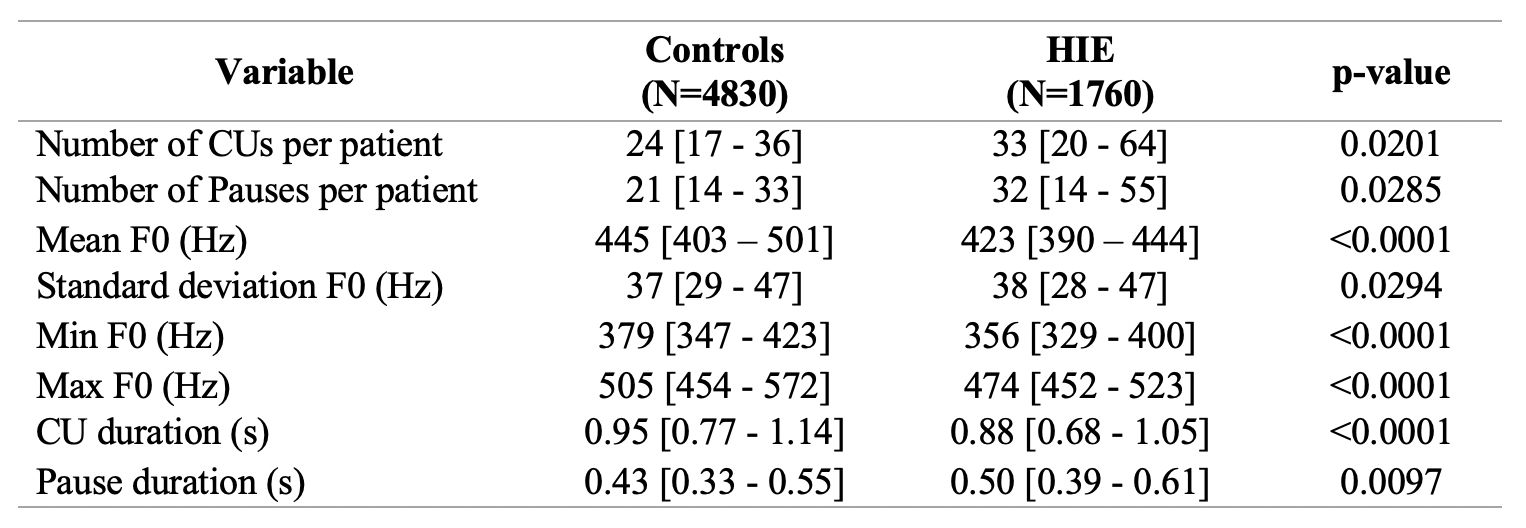
Design/Methods: Infants ≥36wks gestational age and birth weight ≥1800g with history of perinatal hypoxic ischemic insult, transferred for evaluation and possible therapeutic hypothermia were eligible. Enrolled patients were divided in 4 groups: no HIE, Mild, Moderate or Severe HIE by modified Sarnat score at admission. Control infants were enrolled from the newborn nursery. All infants had cries collected for 30sec-3min using an in-house developed smartphone study application during standard care on the day of discharge from the nursery or NICU. The modified Sarnat was also performed at discharge. Cries were manually segmented into Cry Units (CUs; one voiced expiration) and Pauses (time between CUs). From each CU, the mean, standard deviation, min, and max of the pitch (F0) were extracted using an automated algorithm and compared between controls and any HIE (Mild, Moderate, or Severe) as primary outcome. As secondary outcomes, subgroups were analyzed comparing controls with different levels of HIE at admission (Mild and Moderate) and discharge (Normal and Mild).
Results: Cries were analyzed from 171 controls (4830 CUs) and 39 newborns with HIE (1760 CUs). Patient demographics were significantly different between the groups (Table 1). All acoustic biomarkers were significantly different between groups (Table 2; Figure 1A). Compared to controls, the HIE group had lower F0, higher variability in F0, and shorter CUs with longer pauses. Differences in acoustic biomarkers at discharge of Mild HIE were found when compared to control and Moderate groups (Figure 1B). Additionally, HIE patients discharged with a Normal Sarnat have significantly lower acoustic biomarker values than controls (Figure 1C).
Conclusion(s): Acoustic biomarkers are significantly different between healthy newborns and those with HIE. Interestingly, cry analysis of infants with Mild HIE at admission or discharge was significantly different than controls and HIE patients with normal Sarnat exam at discharge, raising concerns about brain injury in this group. Furthermore, differences between healthy controls and HIE patients discharged with Normal Sarnat indicate that acoustic biomarkers may be more sensitive to detect neurological injury; this requires confirmation with upcoming brain MRI results and neurodevelopmental outcomes at 2 years old.