Emergency Medicine: All Areas
Emergency Medicine 1
28 - Emergency Department Prediction Model for Evaluation of Multisystem Inflammatory Syndrome in Children
Publication Number: 28.11

Lauren Chavanne, BS (she/her/hers)
Medical Student
Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo
Orchard Park, New York, United States
Presenting Author(s)
Background: Soon after the initial spread of COVID-19, cases of a post-infectious inflammatory disorder of children (multi-system inflammatory syndrome in children or MIS-C) were reported worldwide. Due to the multisystem inflammation, the workup of MIS-C necessitates a broad range of laboratory investigations. As the symptoms (fever, rash, adenopathy) are commonly seen during infections, rheumatologic presentations, and Kawasaki disease, frontline providers face a dilemma on the decision to perform a broad range of labs (ferritin, d-dimers, etc.) on many children with fever which adds unnecessary cost and delays time to disposition.
Objective: This project sought to provide pediatric emergency medicine providers with a data-based tool to guide the decision to perform more extensive evaluations and guide disposition after initial screening labs.
Design/Methods:
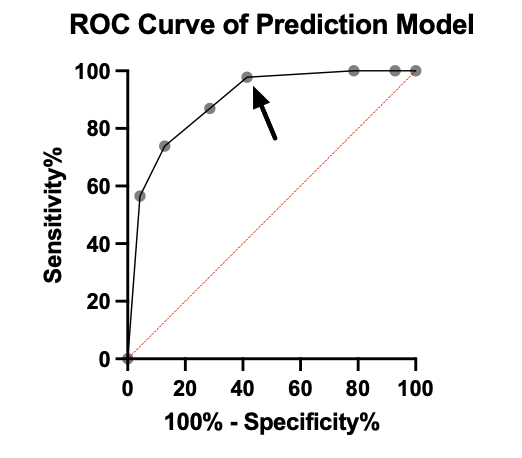
We compared retrospectively collected data from cases of MIS-C to control data extracted from a pre-pandemic database of febrile children. The analysis examined patient data, laboratory data, and primary outcomes to build a model. Initial parameters were chosen using Fisher’s exact test and independent samples t-test. A ROC curve analysis of various parameter collections was used to assess the model’s characteristics. The AUC was used to measure how well the model performs in discriminating between patients with MIS-C and patients without MIS-C to set scoring matrices.
Results:
The analysis included 51 patients with MIS-C and 144 pre-pandemic febrile controls. On initial univariate analysis, age, bilirubin, WBC count, lymphocyte count, platelets, and CRP were all associated. For simplification of workflow, we analyzed a score based on CRP and CBC values. The score demonstrated a sensitivity of 97.83%, specificity of 58.57%, PPV of 60.81%, and NPV of 97.83%. The AUC was 0.89 (95% confidence interval 0.84 to 0.95, p-value < 0.0001). When stratified by age less than 9 years old, the score demonstrated a sensitivity of 96.15%, specificity of 78.57%, PPV of 62.50%, and NPV of 98.21%. When the score was applied to those with MIS-C older than 9 years old, the score demonstrated a sensitivity of 100.00%, specificity of 58.57%, PPV of 40.82%, and NPV of 100.00%.
Conclusion(s):
The scoring system demonstrated usefulness in distinguishing patients with MIS-C from other febrile children. Using this tool, extensive lab evaluation and extended observation of children can be focused on a relatively small subset of patients with first-pass consideration of MIS-C. External validation is needed to verify our findings.