Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 1: Epi/HSR Equity
625 - Neighborhood deprivation does not predict neurodevelopmental impairment at two years corrected age for extremely preterm infants when accounting for covariates
Publication Number: 625.14

Cherise Brackett, MD
Fellow
University of Virginia School of Medicine
Charlottesville, Virginia, United States
Presenting Author(s)
Background: Disparities in healthcare driven by poverty, access to care, and the lasting impact of structural racism impact pregnancy outcomes and child development. Extremely preterm infants (EPT, born at < 29 weeks’ gestation) face neurodevelopmental impairment (NDI) as a complication of prematurity, and sociodemographic factors may exacerbate NDI risk. The Area Deprivation Index (ADI) is a validated, national measure of neighborhood disadvantage that uses census data on income, education, employment, and housing quality.
Objective: Using a multicenter cohort representing different US regions, determine if ADI, measured at the time of neonatal intensive care unit (NICU) admission, is a predictor of 18 - 26 month neurodevelopmental outcomes in EPT infants.
Design/Methods:
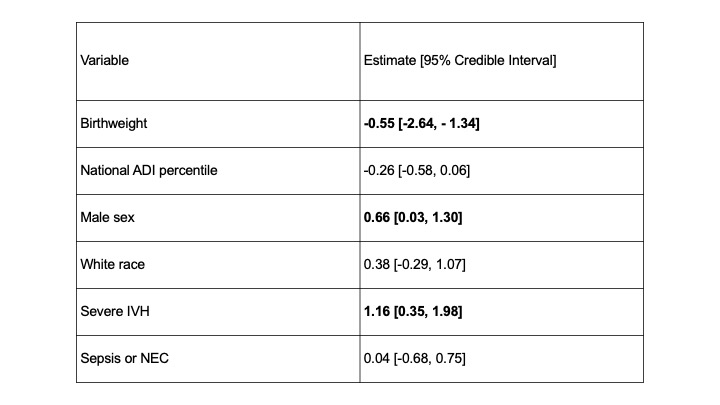
We conducted a retrospective cohort study in 3 level IV NICUs of Non-Hispanic White and Black EPT infants with Bayley’s Scale of Infant Development exams performed at 18 - 26 months corrected age. We converted maternal addresses recorded in the birth encounter to census blocks, identified by 12-digit Federal Information Processing Series (FIPS) codes. The national ADI percentile was then identified for all FIPS codes. We analyzed the relationship between ADI and severe neurodevelopmental impairment (NDI, Bayley score < 70 for cognitive, language, or motor exams) using Bayesian logistic regression adjusted for race, sex, birthweight, severe intraventricular hemorrhage (sIVH, grade III-IV), and sepsis (positive blood culture and ≥5 days antibiotics) or necrotizing enterocolitis (NEC, Bell’s stage 2-3). Predictors were considered significant if the 95% Credible Intervals excluded zero. With standard scaling of continuous variables, we determined the relative importance of predictors by the absolute value of their coefficients.
Results: We studied 236 EPT infants with median GA 26 weeks and BW 830g. In univariate analysis, birthweight and sIVH were associated with severe NDI (Table 1). National ADI percentiles did not differ for infants with and without any NDI (Figure 1). In a multivariable model, birthweight, sIVH, and male sex were statistically significant risk factors, while ADI, sepsis or NEC, and race were not (Table 2). Severe IVH was the strongest predictor of severe NDI.
Conclusion(s): Among preterm infants < 29 weeks’ gestation admitted to three NICUs, birthweight, brain injury, and male sex, but not neighborhood deprivation at the time of NICU admission, were associated with an increased risk of severe NDI. .jpg)
ADI_hist_ndi.jpeg
