Neonatal General
Neonatal General 3: Ethics, Parents Take the Lead
294 - 2012-2021: Increasing Length of Stay Factors for 33 Week Gestation Preterm Infants
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 294
Publication Number: 294.132
Publication Number: 294.132
Kevin Pham, University of Hawaii, John A. Burns School of Medicine, Honolulu, HI, United States; Lauren Muraoka, University of Hawaii, John A. Burns School of Medicine, Mililani, HI, United States; Pattaraporn T. Chun, Kapi'olani Medical Center for Women and Children, Honolulu, HI, United States; Lynn M. Iwamoto, University of Hawaii, John A. Burns School of Medicine, Honolulu, HI, United States

Lauren Muraoka (she/her/hers)
Medical Student
University of Hawaii, John A. Burns School of Medicine
Mililani, Hawaii, United States
Presenting Author(s)
Background: Preterm births in the United States have increased significantly every year. The level of complexity of care required to achieve good outcomes for these infants also continues to accelerate. These factors have contributed to the increasing utilization of healthcare resources and costs. Studies have shown an increase in length of stay (LOS) for very preterm infants across all gestations and types of NICU units. However, the reasons for this increase are not known.
Objective: This study aims to identify antenatal and postnatal factors that correlate with an increased LOS in this population. We hypothesize that factors related to feeding are the major contributors to increased LOS in preterm infants born at 33 weeks gestational age (GA) in 2021 compared to those born in 2012.
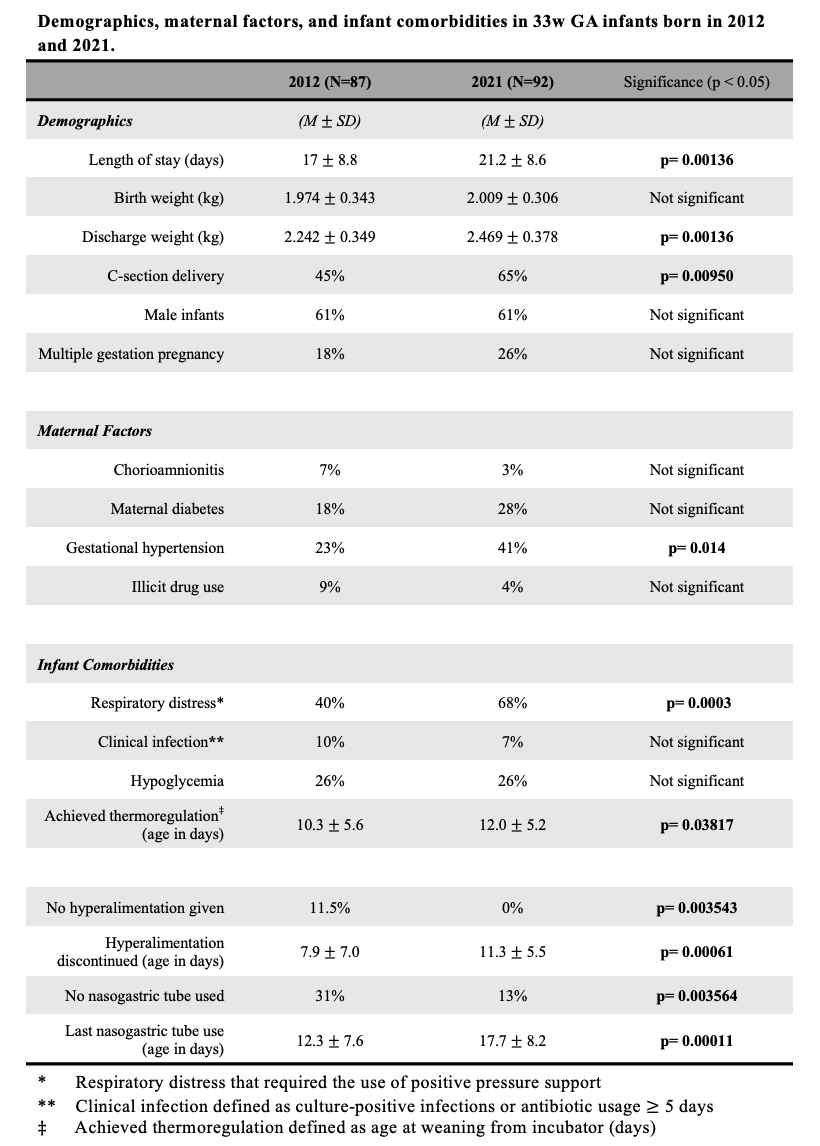
Design/Methods: Retrospective chart review of 179 preterm infants born at 33w0d-33w6d GA who were admitted to KMCWC NICU in 2012 and 2021. Patients with major congenital anomalies, those who did not survive until discharge, and those who were transferred to another facility were excluded from this study. Demographic information, maternal risk factors, and infant comorbidities were collected. The two cohorts were compared by t-test for continuous variables and by chi-square analysis for categorical data.
Results: Infants born in 2021, when compared to those born in 2012, had a longer LOS (21.2±8.6 vs 17.0±8.8 d). A larger proportion of the 2021 cohort were born to mothers with gestational hypertension (41% vs. 23%) and were delivered by C-section (65% vs. 45%). However the rates of maternal gestational diabetes were not different (28% vs 18%). Postnatally, infants in 2021 had a higher need for respiratory support, parenteral nutrition and tube feeding supplementation. When needed, the duration of parenteral nutrition and tube feeding were both significantly longer for the 2021 infants. This cohort also achieved thermoregulation later (12.0±5.2 vs. 10.3±5.6 d) and were larger at discharge (2.469±0.378 vs. 2.242±0.349 kg). (see Table).
Conclusion(s): We found that both antenatal and postnatal factors were associated with the increased LOS for infants born in 2021 vs 2012. Gestational hypertension and C-section delivery suggest that the 2021 infants experienced a greater degree of prenatal stress. Postnatally the 2021 infants required more positive pressure support, more parenteral nutrition, more tube feeding, and longer incubator support. The next step is to include a larger sample size over serial time periods and gestational ages to delineate if the associated factors are due to changes in infant maturity or management strategies.