Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 1: Epi/HSR Equity
624 - Location, Location, Location: The Association Between Neighborhood Environmental Factors And Very Low Birthweight Infant Care Processes And Outcomes
Publication Number: 624.14

Sheila Razdan, MD, MPH (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background:
Racial and ethnic disparities in neonatal outcomes are well-documented. Other areas of health care suggest that neighborhood social and built environment factors may influence health outcomes. National organizations call for including social factors in neonatal intensive care unit (NICU) performance assessments.
Objective:
Describe the contributions of maternal neighborhood factors to four quality-sensitive outcomes for very low birth weight (VLBW) infants.
Design/Methods:
This prospective cohort study included VLBW infants born 2008-2011 from 119 NICUs in the California Perinatal Quality Care Collaborative (N=17,782). Maternal addresses were geocoded and linked to 2010 census tract data on social and built environment attributes from the California Neighborhoods Data System. We used multivariable hierarchical regression including infant, maternal, hospital, and neighborhood factors. Outcomes were high growth velocity (GV), healthcare-associated infections (HAI), chronic lung disease (CLD), and in-hospital mortality. A p-value < 0.05 was determined to be statistically significant.
Results:
Table 1 describes infant, maternal, and neighborhood characteristics. Among 17,782 infants, 53% had high GV, 12% HAI, 21% CLD, and 6% died. Univariate models showed that neighborhoods with high socioeconomic status were associated with decreased odds of HAI, CLD, and mortality. Neighborhoods with high proportions of minorities or immigrants were associated with slower GV, higher HAI, and higher CLD. In multivariable models, neighborhood factors were not associated with HAI or mortality. High population density and non-urban neighborhoods were associated with high GV; greater street connectivity was marginally associated with increased odds of CLD (Image 1).
Conclusion(s): After adjustment for potential confounders in fully-adjusted models, there was a reduction of significant associations between neighborhood factors and VLBW outcomes. The impact of population density and street connectivity requires further investigation. The lack of significant associations of neighborhood factors with HAI supports its use as a unit-specific care process measure; the lack of associations with mortality suggests the NICU environment may buffer the impact of neighborhood influences. Future studies should examine the hypothesis that maternal and infant factors may mediate the relationship between neighborhood factors and VLBW outcomes.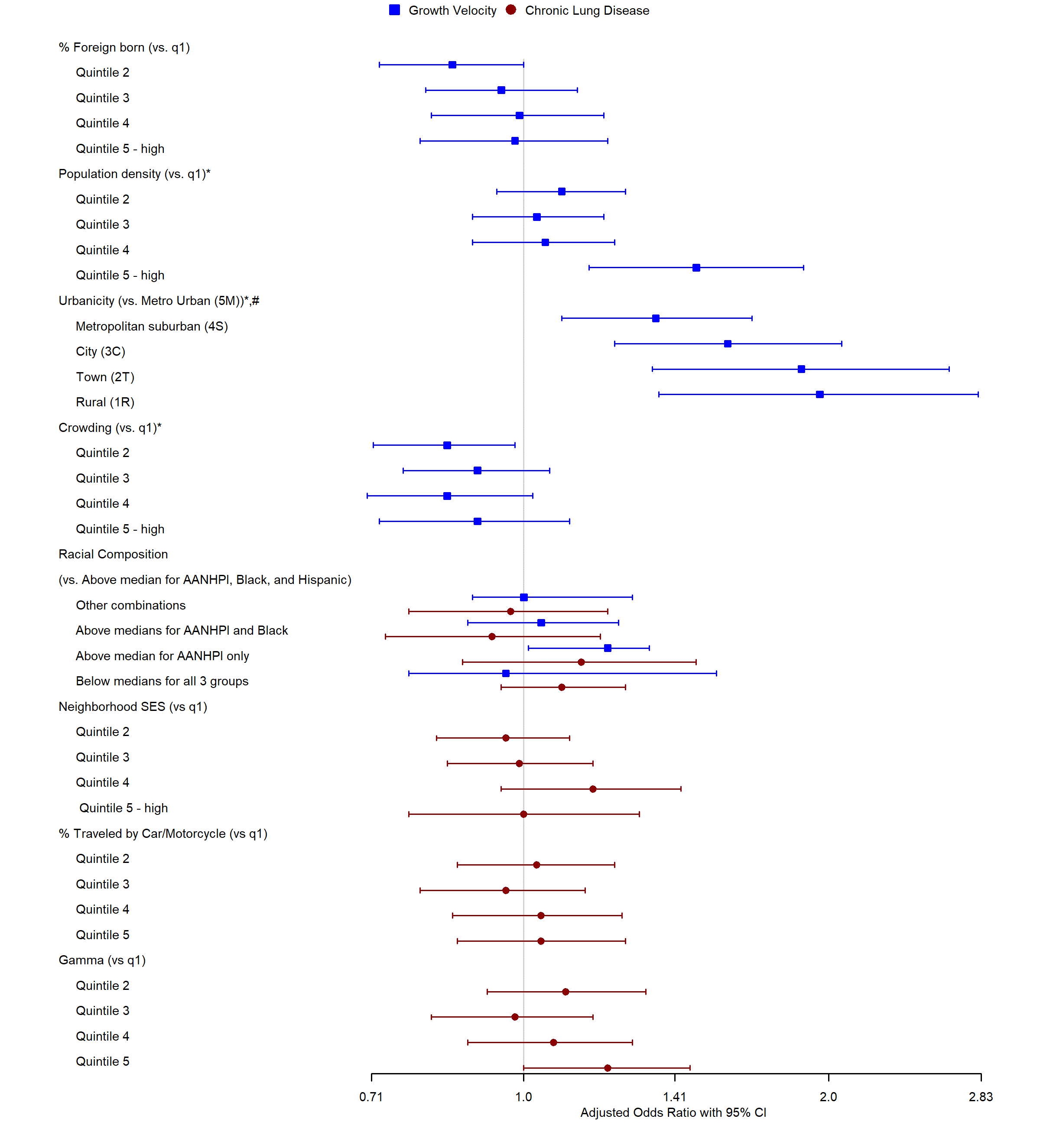
.png)
