Neonatal Follow-up
NICU Follow Up and Neurodevelopmental 2: Neonatal Growth, Nutrition and the Brain
217 - Association of Growth Trajectories with Future Blood Pressure and Mediating Role of Current Adiposity Distribution in Adolescents Born Preterm with Very Low Birth Weight
Publication Number: 217.144

Andrew M. South, MD, MS (he/him/his)
Associate Professor
Wake Forest School of Medicine of Wake Forest Baptist Medical Center
Winston Salem, North Carolina, United States
Presenting Author(s)
Background:
Abnormal catch-up growth in youth born preterm or with very low birth weight may increase risk of developing hypertension. It remains unknown which patterns of abnormal catch-up growth confer this risk and if development of abnormal adiposity distribution is actually responsible for this perceived risk.
Objective: Investigate if early-life growth trajectories are associated with risk of high blood pressure and if adiposity distribution mediates this relationship in adolescents born preterm with very low birth weight.
Design/Methods: Analysis from the Prenatal Events-Postnatal Consequences study, a prospective cohort of 176 individuals born preterm (< 37 weeks’ gestation) with very low birth weight (< 1.5 kg). Youth with major congenital anomalies, genetic syndromes, or major health conditions were excluded. Perinatal data and growth parameters at birth, neonatal intensive care unit discharge, and 1 year corrected age were obtained via parental report and review of health records and research databases. Participants’ height, weight, waist circumference, skinfold thickness, DEXA body composition, and blood pressure were measured at 14 years of age. We defined high blood pressure as ≥120/80 mmHg. We calculated weight z-scores at each point in time. Catch-up growth trajectories were estimated using latent growth curve analysis. We estimated total and direct effects of growth trajectories on blood pressure and indirect effects mediated through adiposity distribution at age 14 years using multivariable generalized linear models and causal mediation analysis with a directed acyclic graph-informed adjustment set.
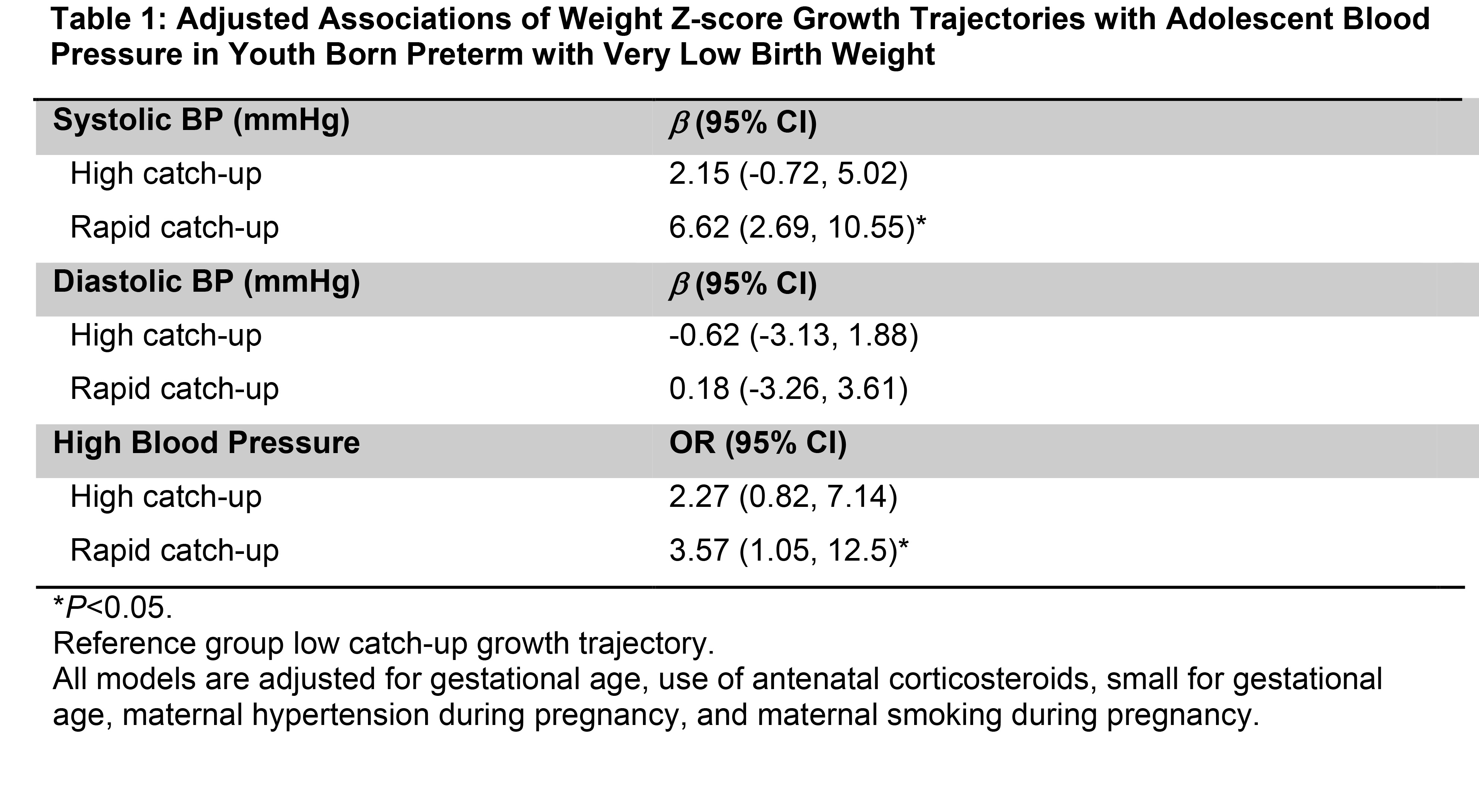
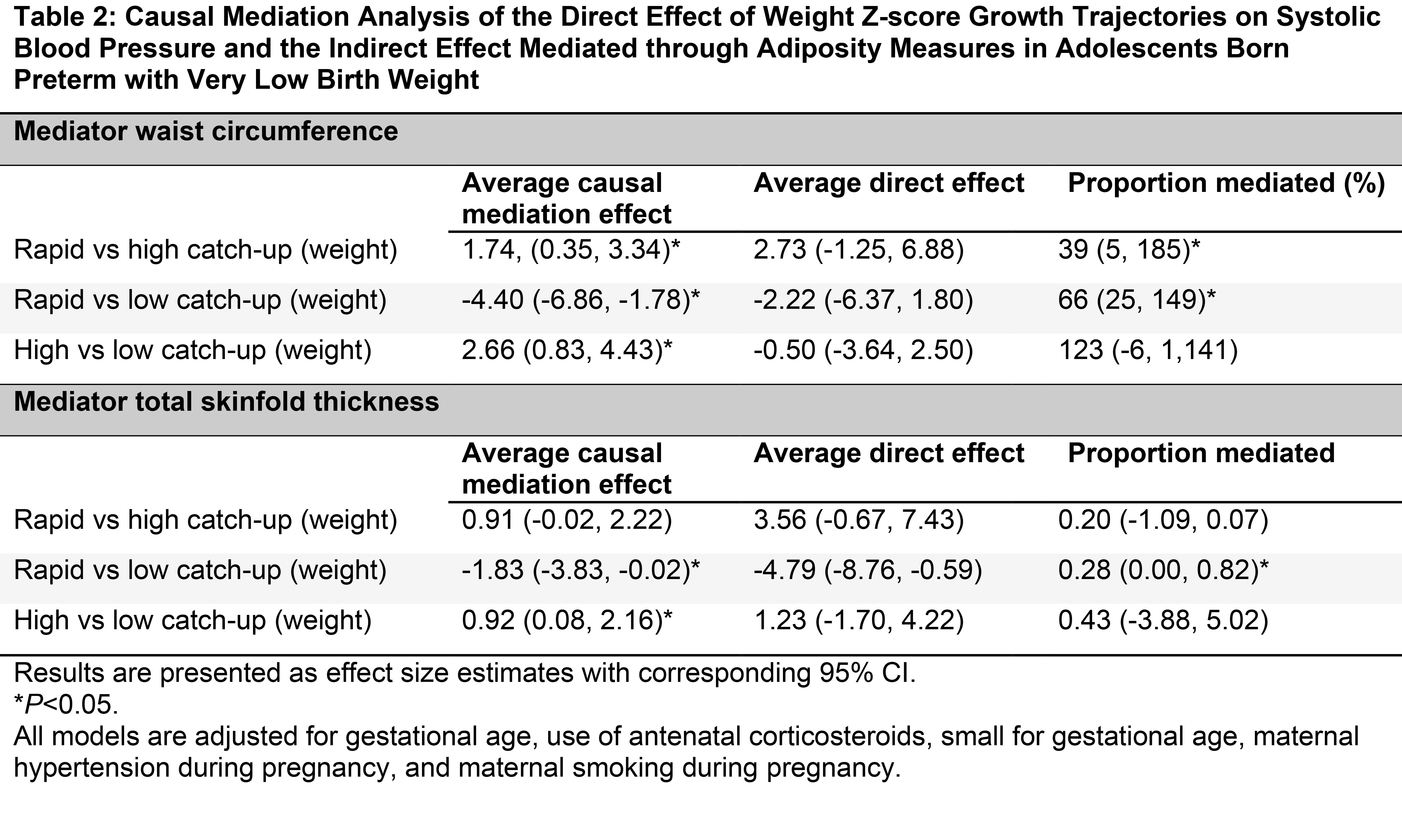
Results: Nineteen percent had high blood pressure. We identified three weight z-score growth trajectories: high catch up (n=86, 49%), low catch up (n=62, 35%), and rapid catch up (n=28, 16%) (Figure). Compared to low catch up, rapid catch up was associated with high blood pressure (OR 3.57, 95% CI 1.05 to 12.5) (Table 1). Measures of abdominal adiposity such as waist circumference and total skinfold thickness mediated 66% (95% CI 25% to 149%) and 28% (95% CI 0% to 82%) of the total effect of catch-up growth in weight z-score on systolic blood pressure, respectively (Table 2).
Conclusion(s):
We observed that abdominal adiposity distribution at 14 years of age mediated the effect of catch-up growth trajectories on blood pressure in adolescents born preterm with very low birth weight. Our results support the idea that later development of unhealthy adiposity distribution and obesity have a relatively greater effect on developing hypertension compared to early-life growth patterns..jpg)