Neonatal General
Neonatal General 2
278 - RDW (Red Cell Distribution Width) Is A Marker For Neonatal Outcome in VLBW Infants
Publication Number: 278.131

Smrithi Madhava Menon, MD (she/her/hers)
Assistant Professor, Neonatology
Amrita Institute of Medical Sciences, Amrita Vishwa Vidyapeetham University
Cochin, Kerala, India
HARJITH HAREENDRANATHAN AJITHA (he/him/his)
FELLOW IN NEONATOLOGY
Amrita Institute Of Medical Sciences
CALICUT, Kerala, India
Presenting Author(s)
First Author(s)
Background:
RDW reflects the variation and dispersion degree of red blood cell volume. Increased RDW suggests significant deregulation of erythrocyte homeostasis due to impaired erythropoiesis or abnormal RBC survival. Factors contributing to this include shortening of telomere length, oxidative stress, inflammation, poor nutritional status, RBC fragmentation and changes in erythropoietin function. There is little information about the association of RDW to prognosis and outcome in VLBW infants.
Objective: We hypothesized that changes in RDW in the first week after birth could be a marker to predict neonatal morbidity. We studied the relationships of serial changes in RDW to the prognosis and outcome of VLBW infants.
Design/Methods: This is a retrospective cohort study of 240 VLBW infants admitted to the NICU (2019-20): mean BW: 1041±378 gms. GA: 28.4±2.4 (23-31) wks. RDW was obtained from the CBC done at birth, day 7, 14 and at the onset of sepsis. Infants who died under 10 days were excluded. The relationships of changes in RDW to BPD, ROP, and late onset sepsis (LOS) and the role of RDW to platelet ratio (RPR) in sepsis were analyzed.
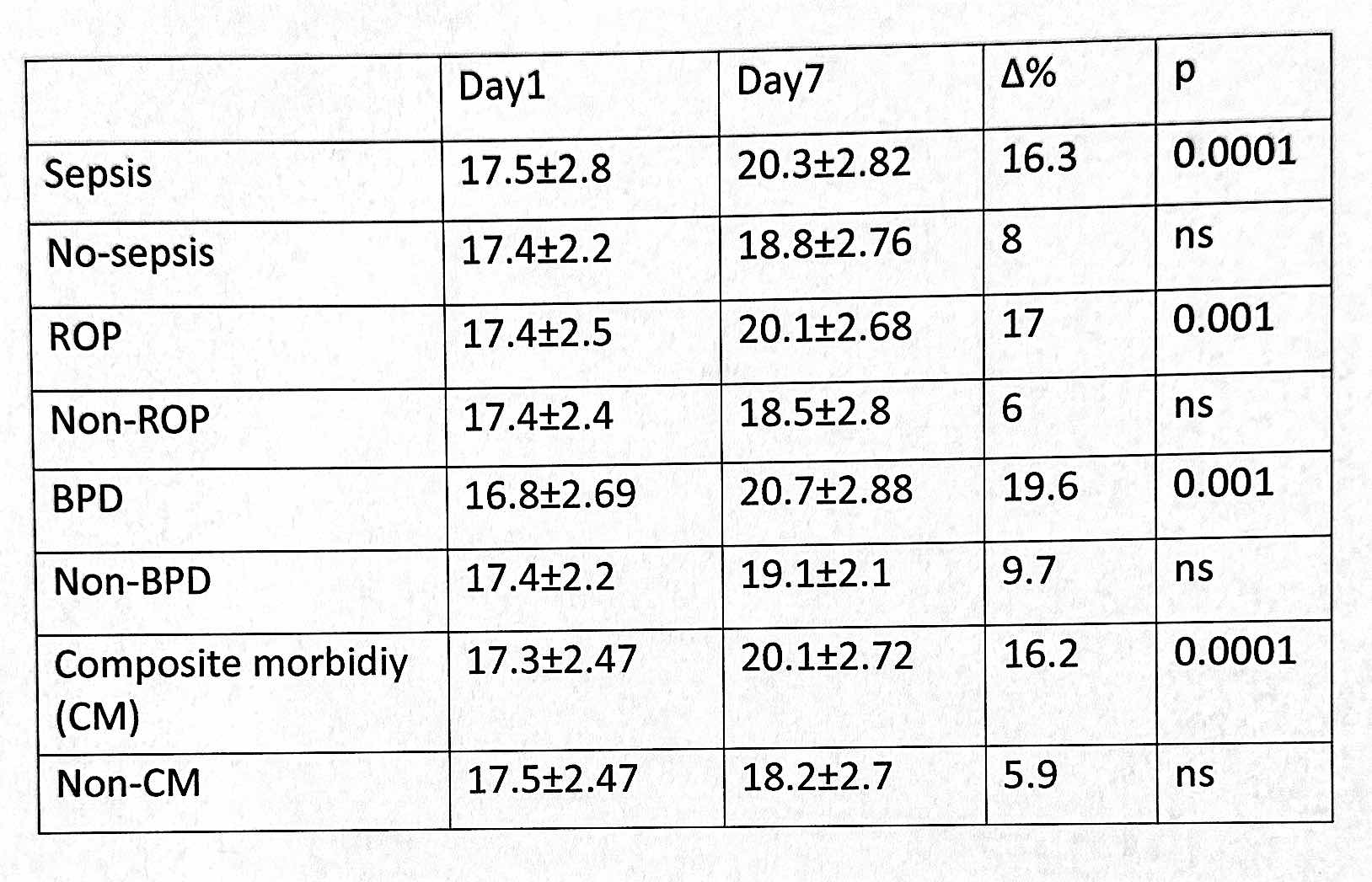
Results: Overall mortality was 13.75%. The incidences: BPD: n=25 (10.4%); LOS: n=76 (31%); ROP (various stages): n= 91 (37%) of which 10 (10.9%) required laser therapy; NEC: n=1 (0.4%).Overall RDW increased from day 1(17.3±2.4) to 7(19.42±3) (p=0.02) and decreased by day 14 (18.41±2.3). The RPR in LOS group was 32.6±28 vs 13.5±25 (p=0.0001) in non LOS. ROP group was further subdivided to ROP+LOS and ROP without LOS groups to avoid the influence of sepsis in ROP. The percent increase in RDW from D1 to D7 was significant in both groups of ROP (with LOS and without LOS) compared to infants without ROP (p=0.001). See table 1.
Conclusion(s):
These results indicate that there is significant increase in RDW postnatally between D1 and D7 in infants who developed BPD, ROP and sepsis. Infants at risk of CM (BPD/ROP/Sepsis) can be detected by the changes in RDW in the first week. Our study suggests that RDW during the first week is a marker for subsequent morbidity in VLBW infants. The mean age of death was 11 days (median 2.5) hence mortality is not included.
We speculate that elevation of RDW from D1 to D7 is a marker for higher morbidity in VLBW infants and might indicate a maladaptive response to oxidant stress in the transition from intrauterine hypoxic state to extrauterine environment which is a predisposing factor for subsequent morbidity. This is a hypothesis testing pilot study, and a larger sample size would be required to confirm these findings and correlate to other morbidities.