Emergency Medicine: All Areas
Emergency Medicine 4
71 - COVID’s Impact on the Treatment and Outcomes of Children with Acute Appendicitis
Publication Number: 71.112

Kelly N. George, BS Allied Health Sciences (she/her/hers)
Graduate Student
University of Connecticut
Coventry, Connecticut, United States
Presenting Author(s)
Background:
The treatment of Acute Appendicitis (AA) has evolved. Traditional treatment includes an appendectomy however non-operative treatment (NOT) with antibiotics is an effective therapy for some children. The COVID pandemic deterred people from seeking care. Combined with provider concerns related to operative management and intubation, little is known about outcomes for children with acute appendicitis.
Objective:
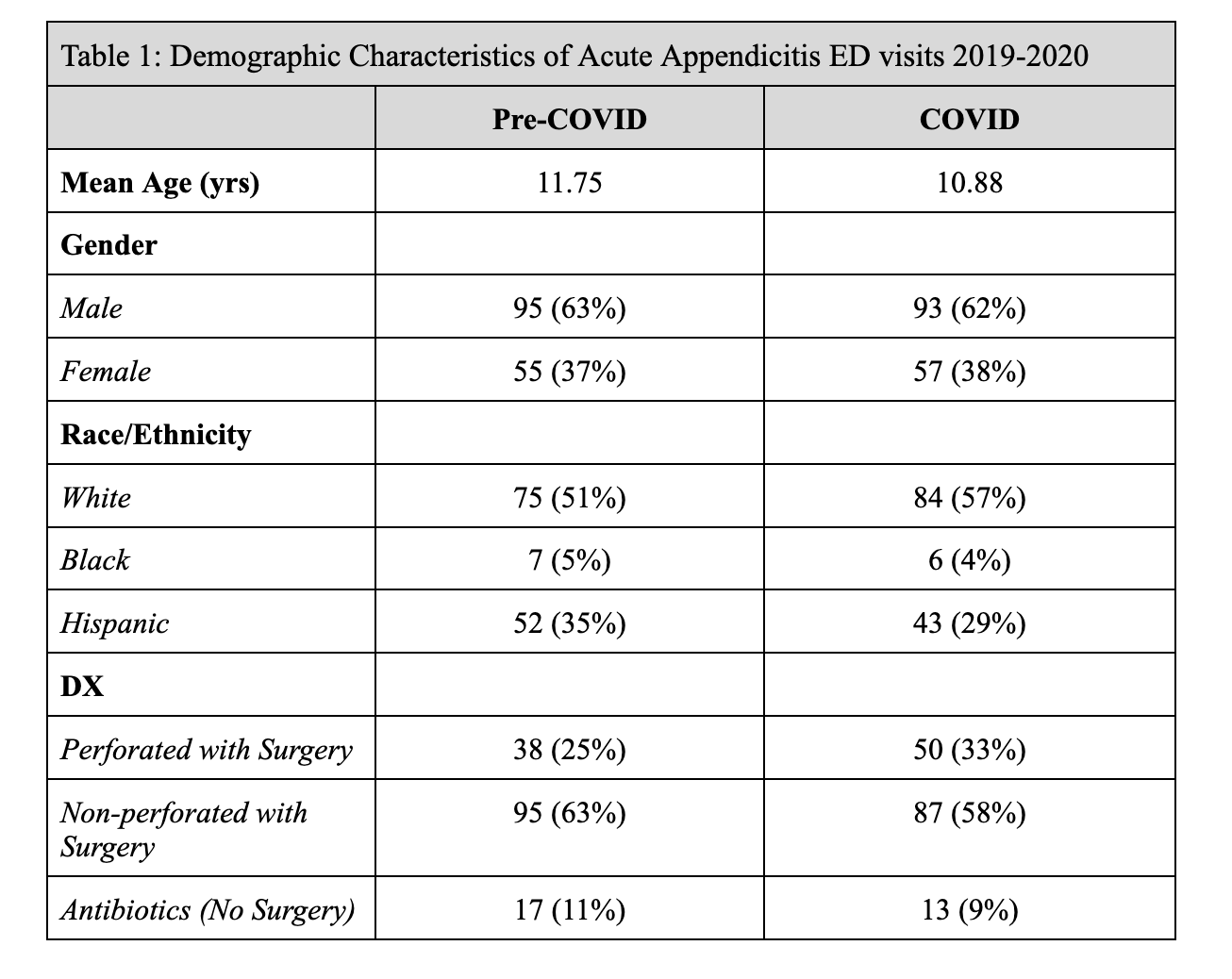
To evaluate the proportion of children admitted for AA before and during the pandemic and associations between operative/NOT, complications, and outcomes. Children preCOVID and COVID were similar with demographics including mean age 11.8 and 10.9 yrs, gender (37%) and (38%) girls, (63%) and (62%) boys, and race/ethnicity (4.8%) and (4.1%) Black, (51%) and (57%) White and (35%) and (29%) Hispanic (Table 1). Imaging modalities were similar between groups. There is no significant difference in children with perforated versus non-perforated appendicitis by year (p= NS). There was also no significant difference in surgery versus NOT. There were so few children with COVID that comparisons were not done. Of the 5 children with COVID and AA, 3 had perforations, 1 received antibiotics and 1 operative repair. The rate of AA increased by 141.3% even though overall ED visits decreased by 47%, p< 0.01. There was a significant increase in the rate of children presenting to the PED with acute appendicitis in the first year of COVID. The diagnostic results and treatment of AA was similar before and during COVID related to demographics, laboratory and imaging studies, and outcomes. There were differences in treatment of AA with fewer receiving antibiotics; however, more children had ruptured appendices. Strong social distancing and mask policies in Connecticut may have impacted the extremely low COVID infection rates in 2020.
Design/Methods: A large children’s hospital EPIC database was queried for those evaluated in the emergency department (ED) for AA in youth aged birth to 25 years in the pre-COVID (March 1, 2019- February 28, 2020) and COVID (March 1, 2020-February 28, 2021) periods. ICD-10 codes were used to identify visits. 300 visits were randomly selected (150 for each study period) and audited for demographic characteristics, laboratories, imaging studies, operative or NOT, perforation rates and length of stay. All COVID positive children were also assessed. Chi-square and t tests were deployed using R and SPSS.
Results:
Conclusion(s): .png)