Neonatal Quality Improvement
Neonatal Quality Improvement 2
668 - Does It Still Hurt?
Publication Number: 668.139

Smitha M. israel, BSN, RN (she/her/hers)
Clinical Program Coordinator
Children's National Health System
Washington DC, District of Columbia, United States
Presenting Author(s)
Background:
During the participation on a QI multi-collaborative project on post-operative pain in the NICU, we discovered that pain reassessments and documentation were irregularly performed. As a best practice we required a pain reassessment within one hour when patients score ≥ 4 on the Neonatal Pain Agitation Sedation Scale (NPASS). As our population is nonverbal, we rely on these assessments to provide effective treatment and pain management.
Objective:
To increase the percentage of pain reassessments for neonates with a previous score of ≥ 4 from 50% to 75% by February 28, 2021 with a global aim of improving pain management for our patients.
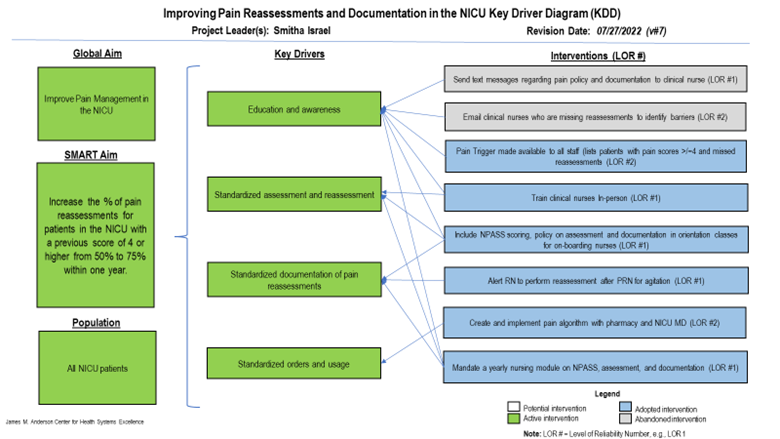
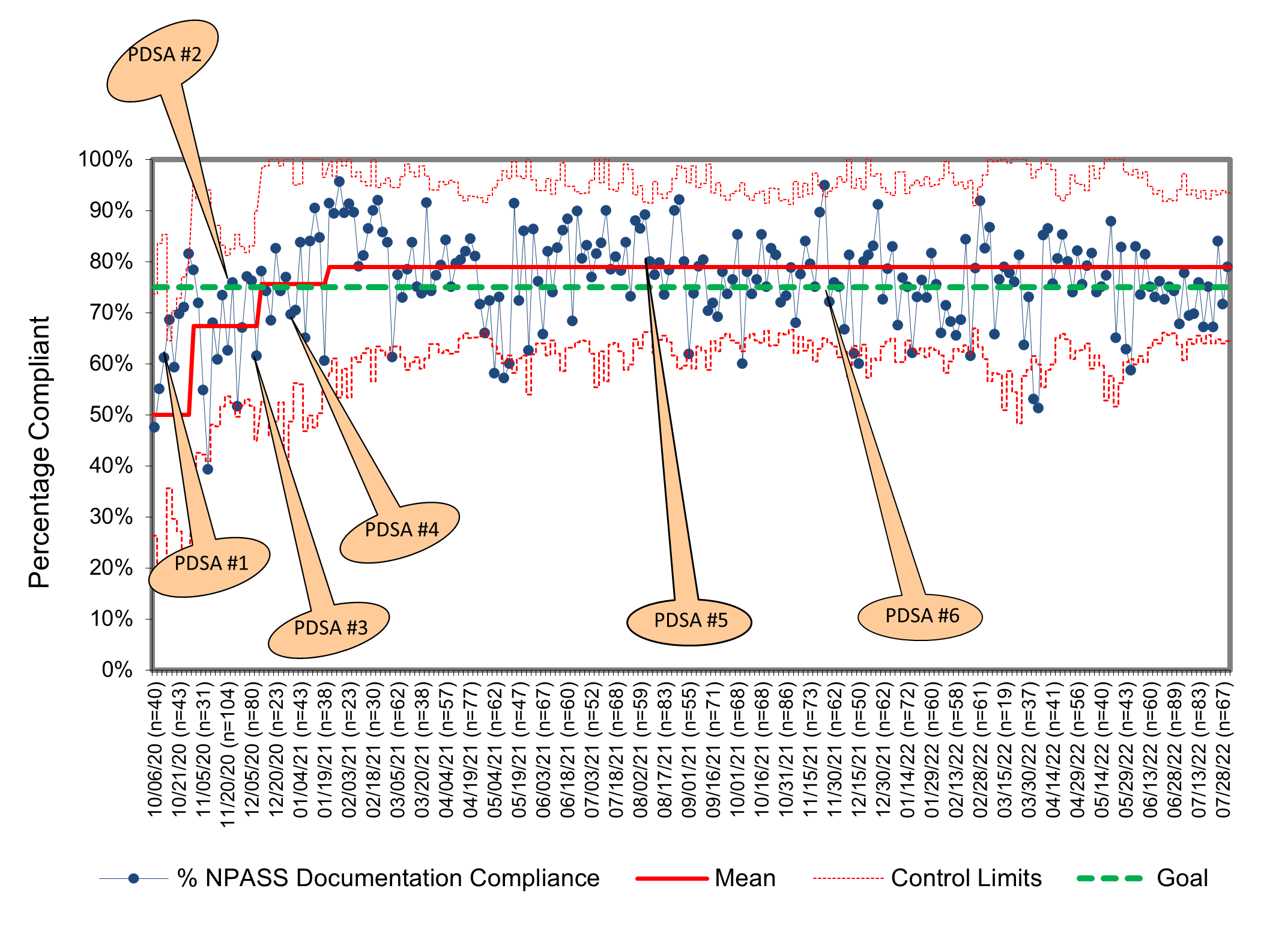
Design/Methods: A QI project to increase reassessments and EMR documentation was implemented over the course of 4 months through multiple PDSA cycles after key drivers were identified. The outcome measure was the rate of patients receiving reassessments within one hour after scoring ≥4 on the NPASS scale. A trigger was developed to produce a daily report on all patients with NPASS scores ≥4. This report provided awareness to noncompliance and aided in the development of interventions. Interventions included reminders to bedside nurses of the hospital policy, real-time feedback of pain reassessments, and more.
Results:
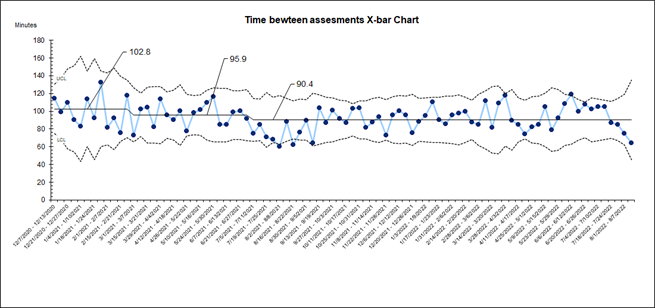
The p-chart showed 50% compliance with pain reassessments with significant variability during the baseline period. This improved to 70% with narrowing variability after implementation of 4 PDSA cycles. With the development of the trigger, we were better able to identify patients with high scores and delayed or missed reassessments. With this report we contacted these specific nurses through different channels to determine their barriers for reassessment and/or EMR documentation. We learned that most of the nurses had simply forgotten to document the reassessment but had completed it. Most frequently this was due to a high workload and high acuity. Later, we were able to see a decrease in time lapse as well as time frame between assessments.
Conclusion(s): In this quality improvement initiative, we determined that a high compliance rate was achieved by staff who frequently performed the reassessment but forgot to document it. Changing culture through persistent reminders should be performed until behaviors change. Future studies should assess the effect of the application of these interventions on pain reassessment and documentation compliance in other units with pediatric surgical and non-surgical patients, the effect of transparent data reporting, and the contribution of workload and acuity on compliance rates.