Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 2: Epi/HSR Equity
638 - Readmission after NICU Discharge: The Importance of Social Determinants of Health
Publication Number: 638.141

John Feister, MD (he/him/his)
Fellow
Stanford University
Palo Alto, California, United States
Presenting Author(s)
Background:
Readmission after discharge from the NICU among very low birthweight (VLBW, < 1500g) infants may be a marker of health risk, healthcare quality, and/or preventable health-system costs. While the social determinants of health (SDoH) influence a wide range of health outcomes, few studies have investigated the roles of the SDoH in risk of readmission after NICU discharge.
Objective:
To determine the associations between SDoH and hospital readmission risk for VLBW infants within 30 days after discharge.
Design/Methods:
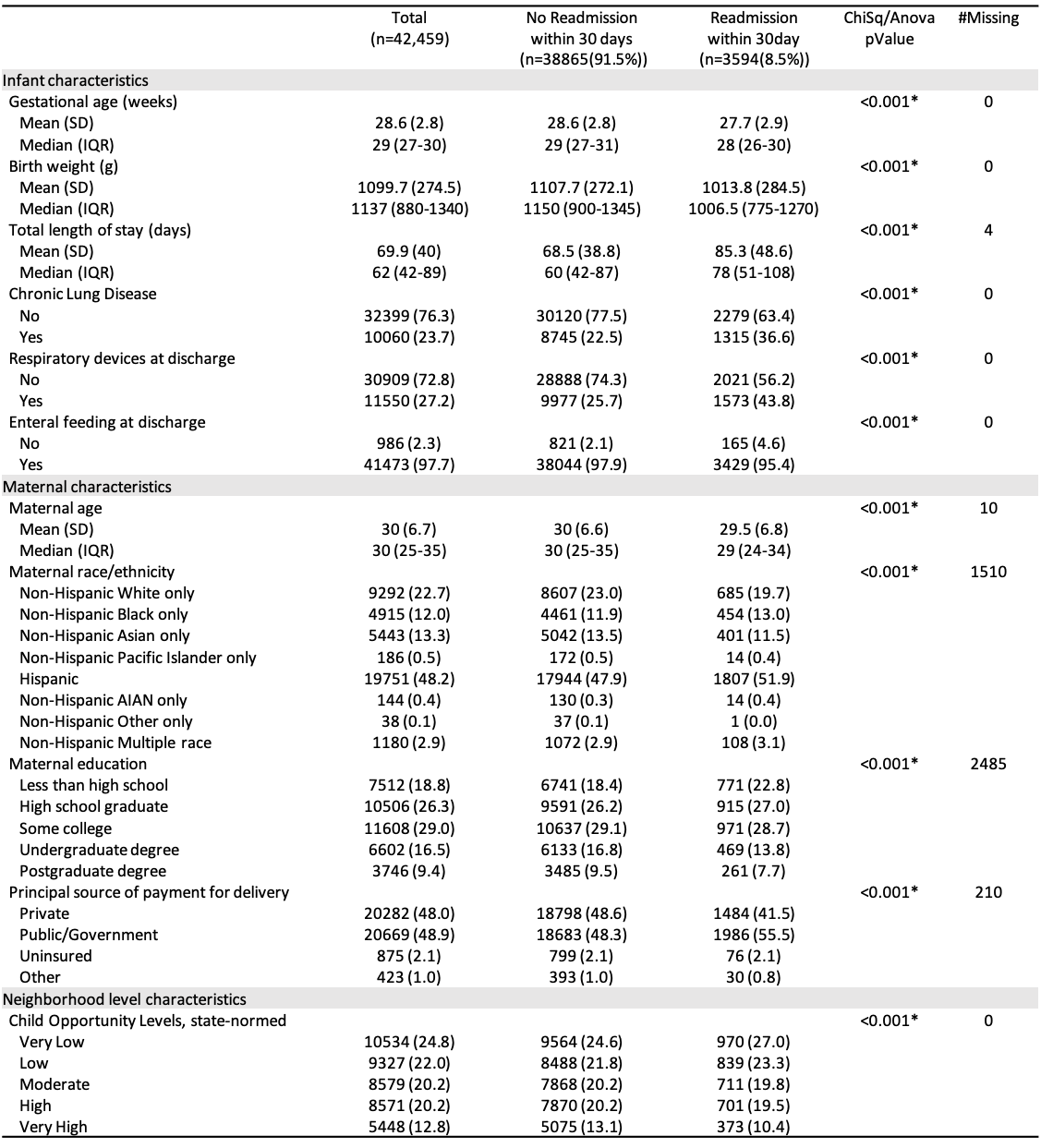
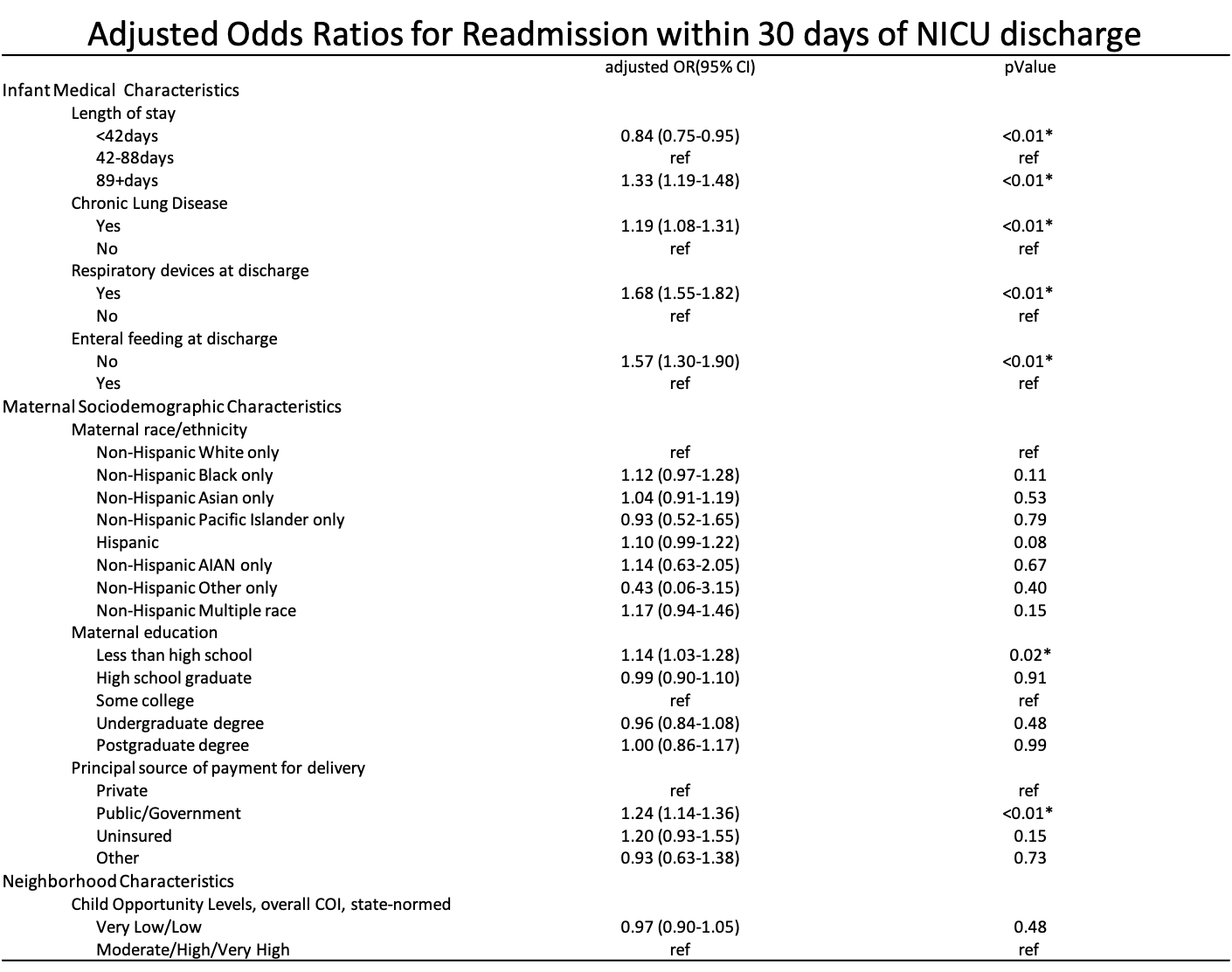
This was an analysis of prospectively collected cohort data from the California Perinatal Quality Care Collaborative (CPQCC), with linkage to California Department of Health Care Access and Information and Child Opportunity Index 2.0. We included all VLBW infants born at CPQCC participant hospitals from 2009-2018. Multivariable logistic regression models adjusting for infant medical characteristics [gestational age, birthweight, length of stay, chronic lung disease (CLD), respiratory devices at discharge (i.e. pulse oximeter or home oxygen), feeding equipment at discharge (i.e. gavage feeds)], maternal sociodemographic characteristics [age, race, education, insurance status (proxy for income)], and neighborhood characteristics [childhood opportunity index (COI) level] were created to estimate odds ratios for hospital readmission risk within 30 days after NICU discharge.
Results:
Of 42459 infants included, 3594 (8.5%) were readmitted. Readmitted vs not readmitted infants differed significantly with regards to infant medical characteristics, maternal sociodemographic characteristics, and neighborhood characteristics (table 1). In multivariable logistic regression models (table 2), the strongest predictor of readmission was medical technology dependence (respiratory devices aOR 1.68, 95% CI 1.55-1.82; feeding equipment aOR 1.57; 95% CI 1.30-1.90). Other medical factors associated with readmission risk included CLD and longer length of stay. Among the SDoH measures, only low maternal education (< HS) and insurance status (public or uninsured) were independently associated with increased readmission risk (table 2). Neighborhood COI was not significantly associated with readmission risk.
Conclusion(s):
After technology dependence, SDoH were significantly associated with VLBW infant readmission risk, with maternal education and income more predictive than neighborhood characteristics.