Breastfeeding/Human Milk
Breastfeeding/Human Milk 2: Addressing Inequities in Lactation
383 - Using Breast Milk From Marijuana Positive Mothers: A National Survey of Neonatal Intensive Care Unit Policies
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 383
Publication Number: 383.102
Publication Number: 383.102
Sarra Bae, University of Maryland Children's Hospital, Baltimore, MD, United States; Natalie Davis, University of Maryland School of Medicine, BALTIMORE, MD, United States

Sarra Bae, DO (she/her/hers)
Neonatology Fellow
University of Maryland Children's Hospital
Baltimore, Maryland, United States
Presenting Author(s)
Background: Marijuana use in pregnant and lactating persons is becoming more prevalent due to both recreational use and pharmacotherapy for conditions such as nausea, anxiety, and depression. Although human milk has significant benefits to neonates, current available literature is inconsistent on the impacts of tetrahydrocannabinol (THC) on the exposed fetus/neonate. Providing appropriate counseling about breastfeeding in THC positive mothers is difficult and inconsistent. Even on a national scale, academic organizations are not unified in their counseling and recommendations. The American Academy of Pediatrics (AAP) states that maternal substance use is not a “categorical contraindication” while the American College of Obstetricians and Gynecologists (ACOG) only recommends abstinence.
Objective: To perform a national survey of neonatal intensive care units (NICUs) regarding their breastfeeding/milk policy for mothers who test positive for THC.
Design/Methods: We surveyed staff at level II-IV NICUs across the country. We obtained data on THC legalization/decriminalization status and background data for each NICU (location, level). We requested their policy for lactation support and provision of human milk based on toxicology screens. We obtained data on: policy for toxicology screening of mother/baby dyads, access to lactation consultants, and effects of THC status on lactation support.
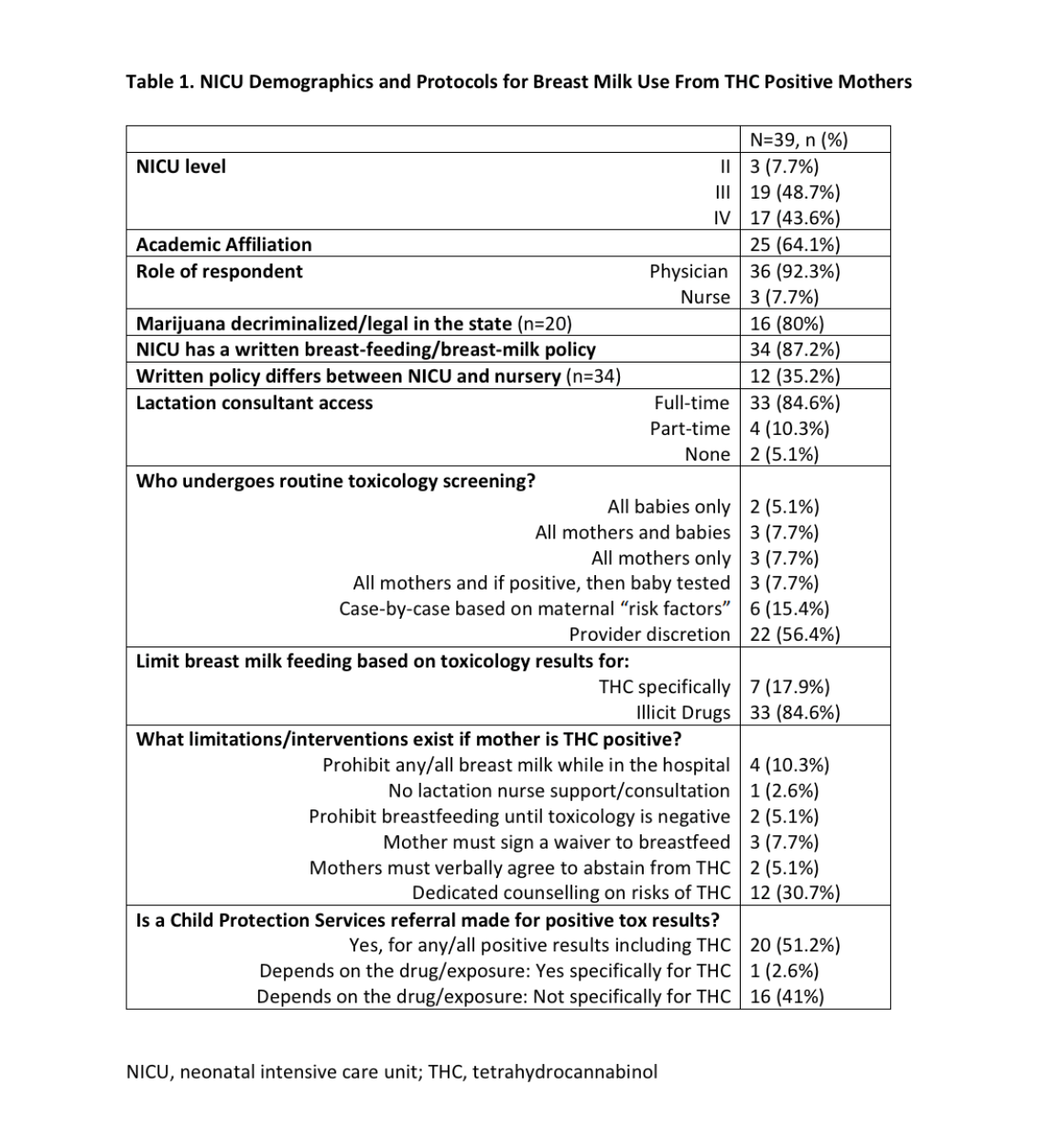
Results: We had 39 responses representing NICUs from 20 states. [Table 1]. Variability existed in who undergoes routine toxicology screening, with ~15% testing all mothers initially, ~8% automatically testing all mothers and babies, and 56% left the decision to provider discretion. When it came to toxicology positive mothers, 87% of institutions may limit breast milk use, with 18% noting they limit based on THC use alone and 85% limit for “illicit drugs.” Limitations in the setting of THC positive status included: 10% prohibiting any/all breast milk use in the hospital, 3% will not providing lactation support/consultation, 8% require mother to sign a waiver to breastfeed/provide breast milk, 5% require mother to verbally agree to abstain from THC use prior to using her breast milk, and 31% specified counselling mothers on risks of THC but allow use.
Conclusion(s): In this preliminary, ongoing national survey of NICUs, wide variation existed in hospital policies regarding toxicology testing for mother/baby dyads, as well on limitations to breastfeeding for mothers who are THC positive. It is important to adopt consistent breast-feeding policies in order to provide consistent care across the nation and limit bias.