Neonatal General
Neonatal General 1: Basic Science and Cardiovascular
261 - Postnatal outcomes of patients with prenatally detected cardiac dextroposition
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 261
Publication Number: 261.13
Publication Number: 261.13
Janani Rajkumar, Oregon Health and Science University, Portland, OR, United States; Emily A. Edwards, Oregon Health & Science University School of Medicine, Portland, OR, United States; Roya Sohaey, Oregon Health & Science University School of Medicine, Portland, OR, United States; Kristey Nguyen, Oregon Health & Science University School of Medicine, Portland, OR, United States; Amanda JH. Kim, Oregon Health & Science University School of Medicine, Portland, OR, United States

Janani Rajkumar, MD (she/her/hers)
Resident Physician
Oregon Health and Science University
Portland, Oregon, United States
Presenting Author(s)
Background: Prenatal diagnosis of cardiac malposition can be associated with intracardiac and/or extracardiac fetal anomalies and warrants additional investigation. Fetal cardiac malposition can be divided into two categories: dextrocardia and dextroposition. Fetal dextrocardia is a type of cardiac malposition where the cardiac axis from base to apex is directed towards the right side. Dextroposition is an abnormal cardiac position, where the heart is shifted into the right thorax, with the apex directed to the left. In dextroposition, extrinsic forces cause cardiac malposition, such as congenital diaphragmatic hernia (CDH), cystic lung malformation, or unilateral pulmonary hypoplasia. Currently, there is limited data regarding postnatal outcomes following prenatal diagnosis of fetal dextroposition in the absence of obvious associated structural anomalies such as CDH.
Objective: The objectives were to determine the ultimate postnatal diagnoses in cases with prenatal dextroposition of uncertain etiology and evaluate the neonatal outcomes.
Design/Methods: This retrospective chart review of patients with fetal imaging at OHSU from 2011-2022 utilized a radiology database and fetal care clinic lists to identify all cases diagnosed with fetal dextroposition and/or dextrocardia. Demographic data, imaging, genetic testing, and postnatal outcomes were collected and analyzed using descriptive statistics. Dextroposition and dextrocardia were often used interchangeably on fetal imaging reports, so while we intended to review only dextroposition, we included patients with isolated dextrocardia as well in our final analysis.
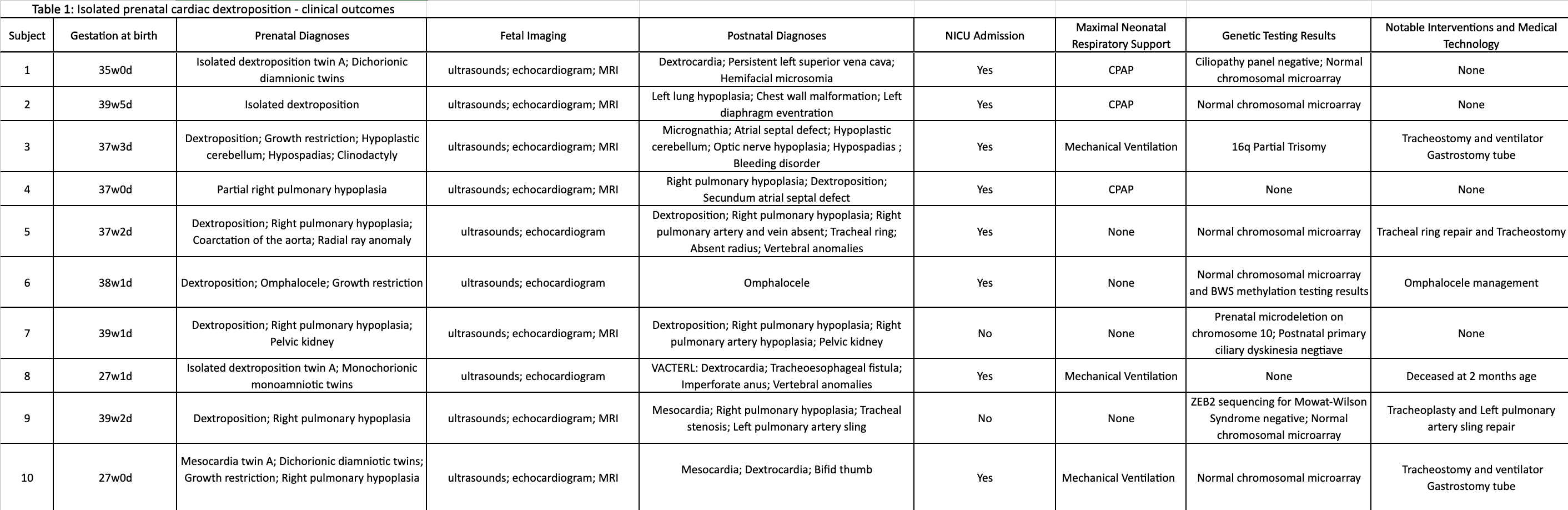
Results: A total of 72 charts were identified with the search terms dextroposition and dextrocardia. Of these, 32 had dextrocardia and 40 were described interchangeably as both dextroposition and dextrocardia. Out of these 72, 10 charts had prenatal findings of dextroposition without clear etiology (Figure 1). These cases were carefully reviewed, with both pre-and postnatal data presented in Table 1. Of these cases, 8/10 required NICU admission after birth, 4/10 had pulmonary hypoplasia as the identified etiology, 3/10 had a clinically significant genetic finding, and 6/10 had additional extra-thoracic anomalies. At a median follow-up of 2.5 years (range 2 months- 8 years), 3/10 children have a tracheostomy.
Conclusion(s): Prenatal identification of dextroposition warrants further prenatal and postnatal evaluation. In our institution’s experience, it is often associated with other anomalies and/or genetic differences as well as a need for a high level of care after birth.
.png)