Quality Improvement/Patient Safety: All Areas
QI 3: Subspecialty-specific QI & Patient Safety
707 - Implementing an Inpatient Postpartum Depression Screening and Community Referral Program in Mothers of Infants with Prenatally Diagnosed Congenital Heart Defects and Prolonged Hospitalizations
Publication Number: 707.153
.jpg)
Juan A. Gallegos, D.O. (he/him/his)
Resident Physician
University of Louisville School of Medicine
Louisville, Kentucky, United States
Presenting Author(s)
Background:
Maternal postpartum depression (PPD) is the leading complication of childbirth. Mothers of infants with congenital heart defects (CHD) are at increased risk for emotional burdens and stressors. Untreated PPD is known to negatively impact the maternal-infant dyad, childhood development, and behavioral patterns. Current recommendations by the American Academy of Pediatrics (AAP) suggests screening mothers for PPD at regular intervals during the infant’s well-child checks. However, infants with complex CHD may require prolonged hospitalizations, making them ineligible from attending their well-child visits, which increases risk for undiagnosed PPD.
Objective:
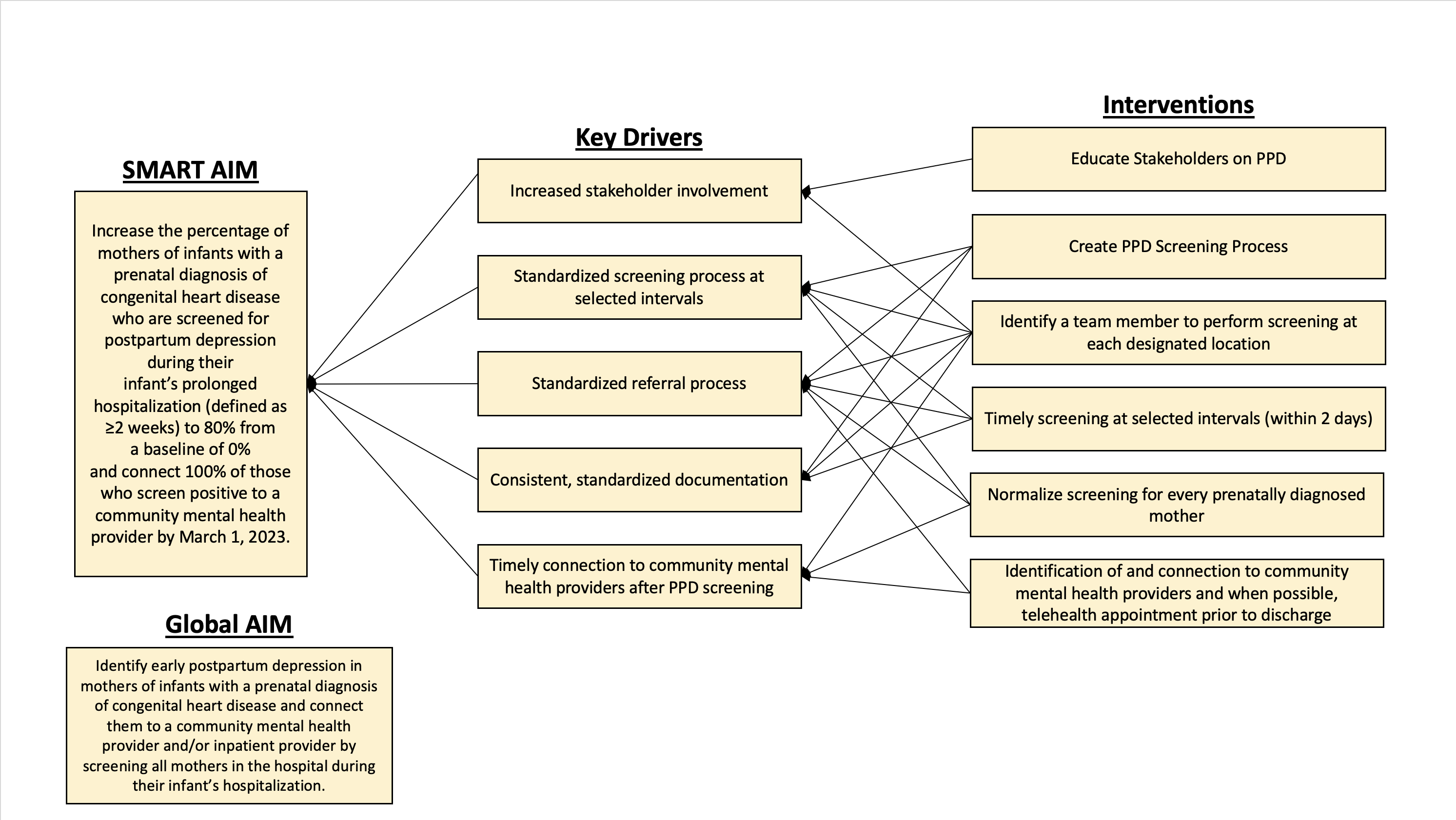
The global aim of this project was to identify mothers of prenatally diagnosed CHD infants with PPD and connect them to mental health resources. Our SMART aim was to increase screening from a baseline of 0% to a goal of 80% and connect mothers with PPD to inpatient and community mental health providers.
Design/Methods:
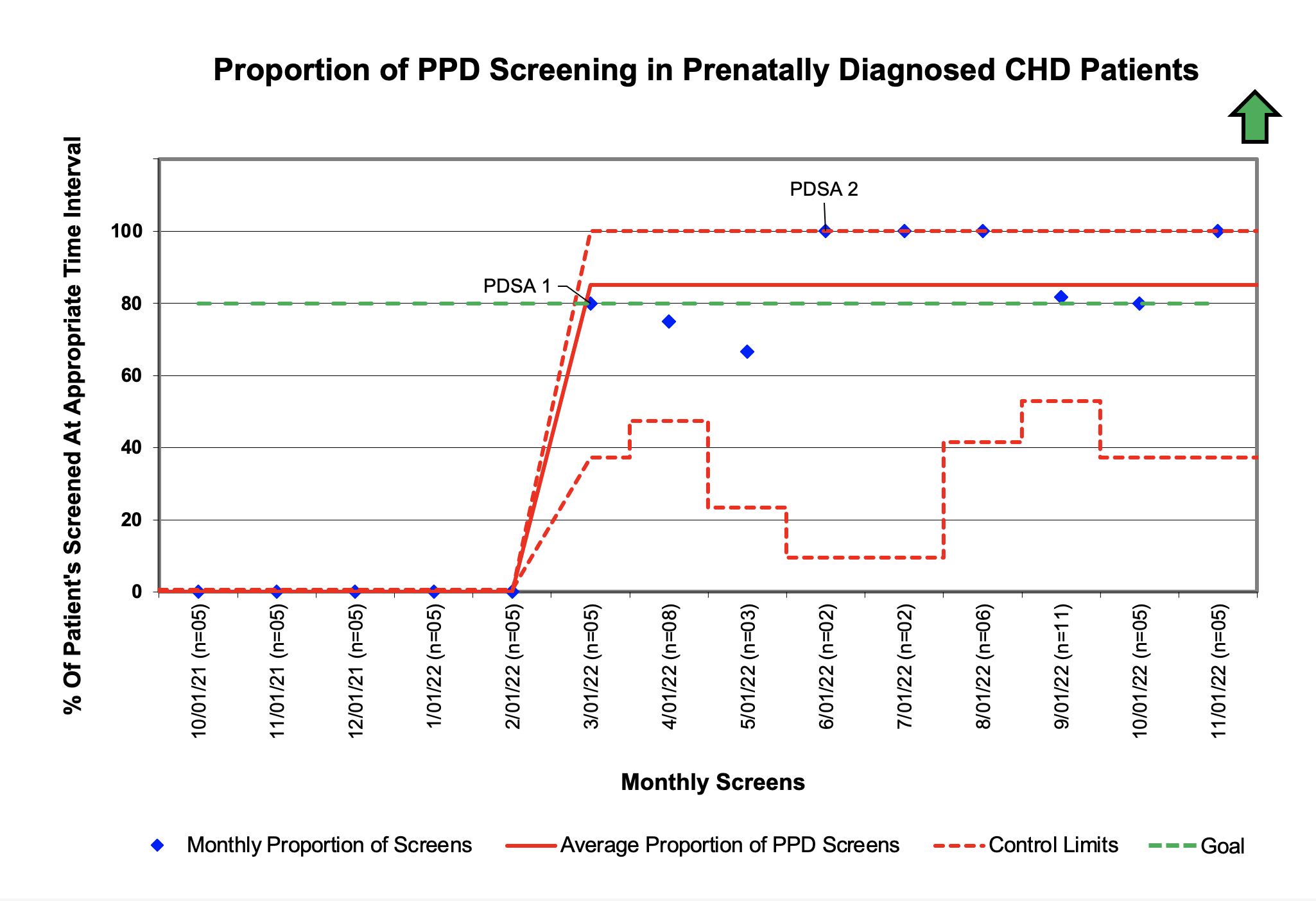
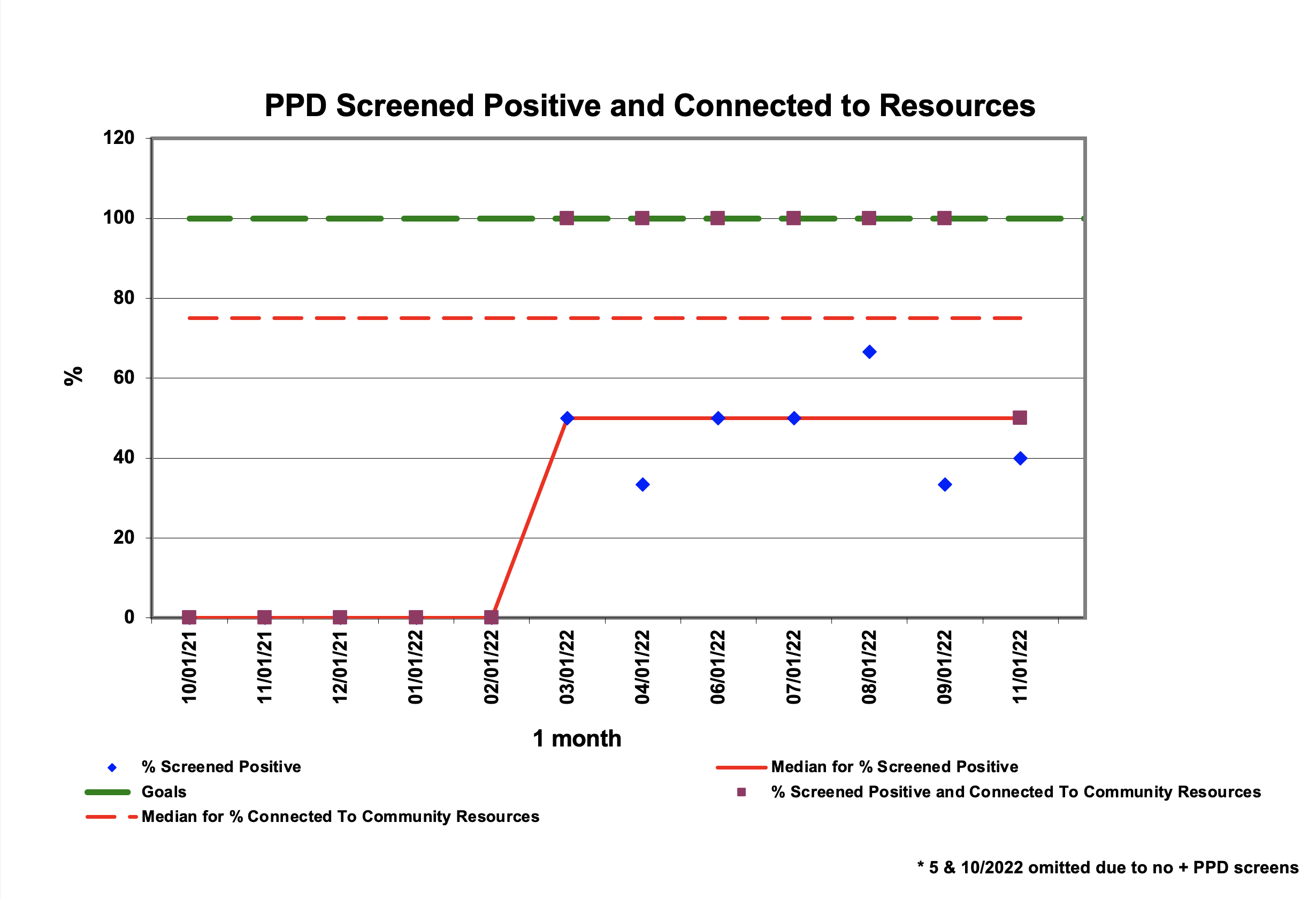
Multidisciplinary stakeholders identified 5 key drivers to impact tests of change. A screening and referral protocol was implemented using the Edinburgh Postnatal Depression Scale (EPDS) at the AAP recommended intervals starting at 14 days postpartum. Mother’s with PPD were referred to our inpatient psychiatry team during hospitalization and to a community mental health provider prior to the infant’s discharge. Our process measure, screening for PPD, was tracked via an annotated statistical process control (SPC) p-chart. Our outcome measure, referral to mental health provider, was tracked via run chart.
Results:
A total of 27 patients were identified to have a prenatally diagnosed CHD. A centerline shift occurred following screening implementation increasing the proportion of mothers being screened for PPD at AAP recommended intervals from a baseline of 0% to 80%. Approximately 46% of mothers had a positive screen on the EPDS. Of those mothers with PPD, approximately 92% were connected to a community mental health provider prior to discharge, 67% opted for additional acute inpatient referral, and 100% were given a provider resource sheet.
Conclusion(s):
Our PPD Screening and Referral Program established a feasible protocol to improve screening and increase referral rates to support maternal mental health. More importantly, it raised awareness of the mental health needs of families highlighting gaps in existing services and referrals. Our program distinguishes itself by connecting mothers with community/outpatient mental health providers thereby ensuring continued support after discharge and ultimately benefitting the mother-infant dyad.