Neonatal Follow-up
NICU Follow Up and Neurodevelopmental 2: Neonatal Growth, Nutrition and the Brain
215 - Body Weight Trajectory in Very Low Birth Weight Preterm Infants and Neurodevelopment Outcomes at 24-month-old Corrected age: a group-based trajectory modeling approach
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 215
Publication Number: 215.144
Publication Number: 215.144
Ts-Ting Wang, Ditmanson Medical Foundation Chia-Yi Christian Hospital, Tainan, Tainan, Taiwan (Republic of China); Yen Ju Chen, National Cheng Kung University hospital, Tainan, Tainan, Taiwan (Republic of China); Yi-Han Su, national cheng kung university hospital, tainan, Tainan, Taiwan (Republic of China); Yun-Hsiang Yang, NCKUH, Tainan, Tainan, Taiwan (Republic of China); WEIYING CHU, National Cheng Kung University Hospital, Tainan, Tainan, Taiwan (Republic of China); Wei-Ting Lin, National Cheng Kung University Hospital, Tainan City CentralWest distinction, Tainan, Taiwan (Republic of China); Yu-Shan Chang, National Cheng Kung University Hospital, Tainan, Tainan, Taiwan (Republic of China); Yung-Chieh Lin, National Cheng Kung University & Hospital, Tainan, Tainan, Taiwan (Republic of China); Chyi-Her Lin, E-Da Hospital, Kaohsiung, Kaohsiung, Taiwan (Republic of China); Yuh-Jyh Lin, National Cheng-Kung U Hospital, Tainan, Tainan, Taiwan (Republic of China)

Ts-Ting Wang, bachelor (she/her/hers)
Fellow
Ditmanson Medical Foundation Chia-Yi Christian Hospital
Tainan, Tainan, Taiwan (Republic of China)
Presenting Author(s)
Background: The survival rate of very low birth weight (VLBW) preterm infants has steadily increased over the past decades, but they remain at high risk of long-term neurodevelopmental impairment (NDI).
Objective: This study aims to evaluate the relationship between post-natal body weight trajectory and neurodevelopmental outcomes at 24 months corrected ages (CA) in the VLBW preterm infants.
Design/Methods: This retrospective study collected data on VLBW preterm infants born at 23-32 weeks' gestation between 2012 and 2017 from the dataset of Taiwan Premature Infant Developmental Collaborative Study Group. Neurodevelopmental evaluations were performed at CA of 24 months. NDI was defined when they had at least one of the following: cerebral palsy, profound hearing loss, profound visual impairment, or cognitive impairment. Body weight (BW) z scores were determined at the time of birth, discharge from the hospital, and 6 months CA by using the Fenton growth chart at birth and discharge, then World Health Organization (WHO) growth measurements at 6 months CA. Three BW z-scores trajectories from birth to 6 months of CA were identified using group-based trajectory modeling. Binary and ordinary logistic regression (LR) were used to identify the risk factors (including growth trajectory) associated with NDI and cognitive, language and motor scales were assessed by Bayley Scale of Infant Development-III (BSID-III) at CA of 24 months.
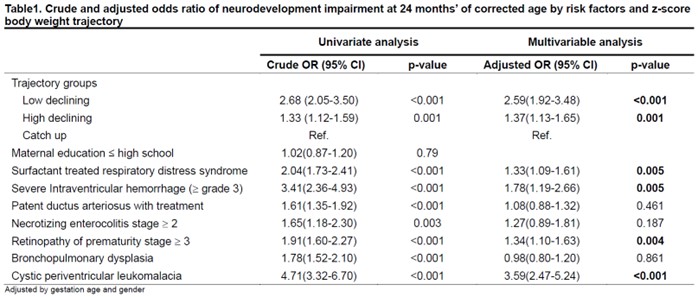
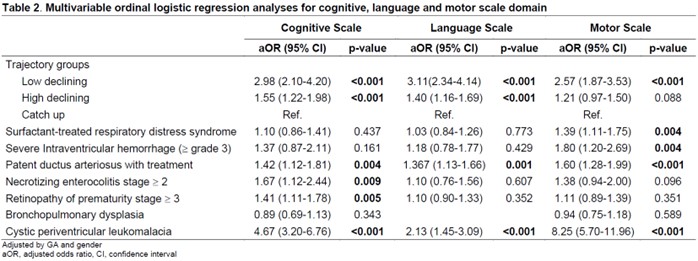
Results: A total of 3581 VLBW preterm infants were enrolled. Three trajectory patterns were classified as catch-up, high-declining and low-declining. Multivariable logistic regression revealed cystic periventricular leukomalacia (PVL) was significantly associated with NDI (adjusted odds ratio(aOR):3.59, 95% confidence interval (CI): 2.47–5.24, p< 0.001) as well as low-declining group (aOR: 2.59, 95% CI: 1.92-3.48, p< 0.001). In the other outcome analysis, mild and moderate-to-severe cognitive, language and motor delays were also associated with the low-declining group and cystic PVL. The aOR in the low-declining group (aOR: 3.11, 95% CI: 2.34–4.14, p< 0.001) was higher than cystic PVL (aOR: 2.13, 95% CI: 1.45-3.09, p< 0.001) in infants with severe language delay.
Conclusion(s): The low-declining group had a significant association with NDI, cognitive delay, and motor delay at CA of 24 months, which was next only to cystic PVL. In addition, the low-declining group had a higher aOR than cystic PVL in infants with lower language composite scale. These findings indicate that growth trajectory within the first 6 months is a risk factor for NDI at CA of 24 months.
.jpg)
